When is Hip Arthroscopy an Effective Course of Treatment?
Arthroscopy is a surgical technique that has revolutionized procedures to solve knee and shoulder joint problems, and these surgeries are performed routinely. Hip arthroscopic surgery is performed much less frequently, because the problems that potentially can be treated this way are much less common. From a technical standpoint, the hip joint is difficult to arthroscope and historically the results of hip arthroscopic surgeries have been much less predictable than with other procedures. As a result, not many orthopedic surgeons even do the procedure. Here’s what a candidate for this type of surgery can expect.
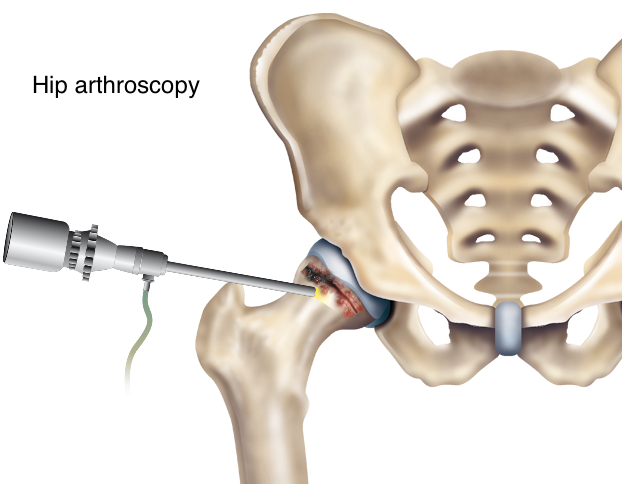
During arthroscopy, an orthopedic surgeon makes two or three small incisions through which pencil-thin, specialized instruments, including an arthroscope, are inserted into the joint. The arthroscope contains a camera lens which magnifies and illuminates the interior joint structure. This information is transmitted by fiber optics to a visual monitor, resembling a TV screen, allowing the surgeon to see the interior of the joint and assess any injury or abnormality that is present. Some conditions can be repaired or corrected by using these specialized surgical instruments.
However, hip arthroscopy is more challenging than knee or shoulder arthroscopy because the hip is located deep within layers of muscle and other important structures such as nerves and blood vessels. To make it easier for the surgeon to visualize the joint, a patient is placed on a special surgical table and traction is applied to the leg being arthroscoped to slightly separate the joint. Nerves potentially can be injured by this traction and care is taken to prevent this.
The beauty of hip arthroscopic surgery is that it is a much less invasive way to solve some hip problems rather than through a large, open incision.
Advantages to hip arthroscopic surgery are:
• Much smaller incisions are made.
• It typically is performed as an outpatient procedure.
• It fosters earlier and accelerated rehab, although depending on what problem is being treated, patients may be instructed not to bear full weight after surgery for a period of time or instructed to wear a hip brace to limit hip motion.
• For many patients, it allows them to return to normal activity faster than if a traditional, open incision procedure is used.
Who is a candidate for hip arthroscopy?
Usually this surgery is selected for people who have hip pain or instability and their hip. X-rays do not show significant arthritis or joint space destruction and often both x-rays and MRI scans only show minimal findings. These symptoms can go on for months to years because the diagnosis is not obvious. Many patients become frustrated and even depressed because they know something is wrong, but diagnosis and treatment are not readily apparent.
What we’ve found is that hip arthroscopy has been most effective in treating conditions which include:
• Impingement: This is when a person experiences pain during full hip movement, because the neck of the femur pinches into the rim of the hip socket. Techniques have been developed to address impingement by removing the excess bone on the rim or femoral neck and then surgically repairing or tacking the labrum back to the rim.
• Labral Tear: A tear in the thick tissue that surrounds the hip socket. The labrum helps to support the hip joint and when a tear occurs, a piece of this tissue can be pinched and cause pain. Note, if the labral tear is secondary to an underlying mechanical problem, then only treating the torn labrum and not the primary cause of the tear might provide temporary relief, but will not solve the problem. Often, patients who develop a labral tear due to impingement and undergo hip arthroscopy don’t do well unless the cause of the impingement also is addressed.
• Loose Bodies: When pieces of cartilage and/or bone break off and remain within the joint. These small, floating pieces can become caught in the hip during movement. This can make you feel as if your hip were locked or stuck and often results in sudden pain. Loose bodies often can be removed arthroscopically.
• Synovitis: When the lining of the hip joint is inflamed and causes pain, it can be partially removed by arthroscopy. This can reduce pain, but it is important not to ignore the underlying cause of the inflamed synovium or the synovitis will return.
• Snapping Hip Syndrome: Characterized by a snapping sensation and sometimes an audible popping noise when the hip is flexed and extended. There are several causes, but most common is when tendons or soft tissue catch on bone and then snap when the hip is moved. The offending tendon on soft tissue can be released or trimmed to relieve this.
• Cartilage Damage: Arthritis is a condition where the cartilage overlying the femoral head or lining of the hip socket is damaged or worn away. Micro fracture is one technique used to slow or stop arthritic progression and encourage healing. Tiny holes are created in the bone that supports the cartilage. This causes the bone to bleed, which stimulates a healing response. Fibrocartilege will grow and cover this area of the bone, and this sometimes can slow the progression of arthritis and relieve pain. Some patients do well; some do not. Your doctor might suggest this procedure, depending on the size and location of the lesion.
As with any surgical joint procedure, there can be complications including infection and continued pain after surgery. A significant concern is with the important nerves and blood vessels that surround the joint. While nerve damage is uncommon, it is important to discuss your particular condition with your surgeon.
Although I routinely perform knee arthroscopy, I do not perform hip arthroscopy. I do, however, see many patients who come to me after they have had a hip scope and are not doing well. These patients require total hip replacements. I recognize that I only see the population that has not done well; many patients greatly benefit from hip arthroscopy. When appropriate, I occasionally refer patients with hip pain to a doctor who performs this procedure.
Arthroscopic hip surgery is new and the indications and techniques still are being defined. Surgeries to treat hip laxity and different types of impingement continue to be refined. These are technically difficult surgeries and their outcomes are less predictable.
My impression is that young patients tend to recover better and more predictably than older patients, primarily because they have less underlying arthritis or cartilage damage. Also, when we are younger, our tissue quality is better and we have more healing potential. Patients with an acute injury that lead to a hip problem, such as a torn labrum, seem to do better than those with less-defined causes and symptoms, or those with long-term conditions.
If an acute injury leads to a problem and it is treatable arthroscopically, then it is to the patient’s advantage to be treated sooner rather than delay the surgery. If a patient has hip dysplasia (on the x-ray, it looks like the femoral head is not fully covered by the socket or acetabulum) and a torn labrum, then hip arthroscopy won’t lead to a good result and I wouldn’t recommend it.
For a young person hoping to avoid a total hip replacement or some other procedure, arthroscopy might be a reasonable alternative. It is important to be fully educated regarding the risks.
Also, make sure you chose a surgeon who has performed a significant number of hip arthroscopic surgeries. Talk frankly with your doctor about his or her surgical success rates as well as the potential success rate for your particular problem.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.












I’m 59 with oesteopenia and arthritis of the hip and they want to do full hip replacement. I don’t have constant pain to the hip but get terrible ‘surprise’ pain at unpredictable times when walking which corresponds to the labrum being pinched or loose labral bodies in there. The ‘attack’ is not consistent with any one particular movement. Like sometimes a torque to the hip while transitioning will do it but sometimes not. The impingement is also from an osteophyte basically where the ‘cam’ of a Femoral Acetabular Impingment morphology would be. Do I have the option of having my hip scoped of the loose labral bodies and cleared of the osteophyte that’s impinging on the labrum. I would still have arthritis but maybe it could be asymptomatic. I just want to ISOLATE what I have good reason to believe is causing the ‘surprise’ attacks to the hip which would be that oesteophyte where the cam deformity usually is, a labral tear and loose labral bodies floating around the hip joint.
Dear Jane,
From what you described, anything less than a total hip replacement will be a disappointment in the long run. It’s possible that you may gain some short-term benefit from undergoing an arthroscopic debridement, but it’s also very likely that it will not help you and actually could accelerate the arthritic destruction. It sounds like you’re developing hip arthritis secondary to an underling congenital malformation leading to CAM acetabular femoral impingement. This is a very common reason why people develop hip arthritis. Your symptoms sound mechanical and probably secondary to labral pathology from the underlying impingement. Arthroscopic debridement of the labrum doesn’t solve the underlying abnormality that lead to the tear and osteophyte, and at best it’s a short-term fix. The reality is that the hip tends to be a more difficult joint to arthroscope than most other joints because it is surrounded by a thick layer of tissue and the joint tends to be tight. This unfortunately can lead to unintentional injury.
There’s also an arduous rehabilitation after a hip scope, because a period of being non-weight bearing and physical therapy is required.
My advice is to avoid an arthroscopy, figure out what exercises and activities you can do that don’t cause pain and delay THR as long as you can GRACEFULLY (or reasonably). When you do capitulate, seek out an orthopedic surgeon who’s really a pro and from whom you get the right vibes.
I wish you only the best,
WAL
Hi, my preteen daughter fell on her hip a year ago, and has finally been diagnosed with a labral separation and also cartilage defects measuring 1×2 cm which go to the bone on both her femoral head and acetabulum. Our doctor has suggested arthroscopic microfracture surgery. Do you think this will be successful for the size of missing/injured cartilage? Also, how can I find info on which doctors/hospitals have the best experience to increase the chances of getting our child walking again? She has not been able to bear weight on her hip since her injury. Thank you.
The goal in treating the hip condition of a preteen or very young adult is to correct the underlying problem and hopefully preserve the natural joint. Every attempt should be made to avoid joint replacement for as long as possible or inevitably. The treatment proposed for your daughter might be the most appropriate and have the best chance for success; I can’t know for sure. There could be an underlying condition that led to the tear and early arthritis, such as hip dysplasia. If the tear and early arthritis occurred because of an underlying mechanical abnormality, then that needs to be corrected first or simultaneously. My recommendation is that you seek opinions from orthopedists who truly specialize in treating hip problems in younger people, such as a physician with a special skill and interest in sports medicine who does hip arthroscopy or a pediatric orthopedist who in comfortable with pelvic or proximal femoral osteotomy.
I wish the best for both you and your daughter as you search for treatment.
Dr. William A. Leone
Hi,
I am 28 and was diagnosed with a label tear a couple of years ago. I have deep narrow sockets. I’ve been putting it off because I was hopeful that physical therapy could help.
While it has helped, it hasn’t been consistently better.
I have excellent range of motion, and I’m functional. But the pain is always there. I am exhausted from being in pain all of the time, and I’m getting muscle imbalances from favoring it.
But I’m also scared to lose my range of motion, develop complications, or have to have subsequent surgeries if it tears free again.
Would you say I’m a decent candidate? Or that waiting it out until I am les functional is smart?
It’s bad, but I’m not crippled. I’d hate to live with it if I knew my decision to have surgery made it even worse.
Dear Daicey,
The threshold to recommend total hip replacement is considerably higher the younger a patient is, because the best and most consistent results are often with the first replacement. With each subsequent revision surgery, the result may not be as perfect or consistent. What has changed for the better is the quality of the bearings, which are used in modern-day hip replacement.
Still, the overall philosophy should be to delay the surgery as long as you reasonably can, particularly considering you’re only 28 years old and still functional. Your description of “deep, narrow sockets” sounds like an “over coverage” condition with your femoral heads seated too deeply within your acetabulum. This is a congenital condition. The labral tear might be secondary to “pincher” type impingement between the femoral head and acetabulum. If your joint space is still and hyaline articular cartilage are still maintained, I would consider being evaluated for a hip arthroscopy with the goal of having the acetabular rim partially reshaped to remove the part of the bony rim that is impinging. Some physicians might also consider a pelvic osteotomy to reposition the socket into a more normal anatomic position.
If these options are not appropriate for you or you decide not to pursue immediate treatment, then I would make lifestyle changes to delay hip replacement until you’re just not happy and actively living the life you want to lead. At some point in your life, hip replacement will be appropriate and hopefully will be life changing.
The best of luck,
Dr. William A. Leone
I am 52 and have osteophytes on my left hip, secondary to acromegaly, that create mild pain and soreness but mean that I cannot walk without a limp, which I am finding very depressing. I still have wide joint spaces and very good (full) range of movement, having been hypermobile even prior to my pituitary condition. The hip problem and walking imbalance I have had for two years now appears to be starting to aggravate the left knee.
Does hip arthroscopy offer any prospect of removing the osteophytes and enabling me to walk normally again?
Hello Ian,
If your symptoms truly are secondary to the development of the osteophytes, then a hip arthroscopy may potentially help. I would be very suspicious that the osteophytes are secondary to underlying osteoarthritis, with the joint space experiencing abnormal joint reactive forces. Usually, the osteophytes (also called bone spurs) are asymptomatic. Occasionally, osteophytes do restrict motion or cause pain when the limb in placed in certain positions resulting in impingement. You report that even now your motion is good.
It’s possible that your abnormal gait pattern is not being caused by hip pathology but another source, including a neurologic compromise (either central or peripheral) from bony overgrowth resulting in impingement or compression of neural elements. It’s critical that the source or etiology leading to your symptoms be found and then efforts made to resolve that problem in order for your symptoms to improve. I think a through neurologic exam indicated.
I would consider discussing with your surgeon a hip injection test. If pain is relieved after the placement of a local anesthetic into the hip joint, and you find you can walk more normally, then it would indicate that you might benefit from a hip replacement. However, you may or may not benefit from a hip arthroscopy. I also would suggest that you discuss with your surgeon the pluses and minuses of having an arthroscopy versus THR. If the arthroscopy fails, it would not preclude you from then having a THR.
I wish you the very best,
Dr. William Leone
Dr. Leon’s, your information and candor to the questions are great! I’m hoping you can offer guidance…I am a 48 year old very active woman with a history of pelvic fracture (ilium and ischium) 30 years ago after accident. I’ve been fortunate that I have been able to maintain my activity level until the last 3 years. After a yoga “incident” and a running incident I am quite debilitated with deep groin pain, Left hip, referred to SI, and piriformis. I cannot fully forward flex, twist, or sit for very long. External and internal rotation are painful. I’m also a yoga teacher and my livelihood is greatly compromised. I sought 2 opinions. One diagnosed trochanter bursitis even though my symptoms aligned greatly with a labral tear. The second doctor has, after 2 failed injections (SI and piriformis) and an MRA confirmed that I do indeed have a labral tear, CAM FAI, degeneration, and narrow joint space. He has ordered one more intra-articular anterior injection. Research has shown that an arthroscope would not have great outcomes for me…I am considering pushing for a THR, because I am completely debilitated. Is that something you would recommend? And what is your opinion of a minimally invasive vs. an open procedure? I’m healthy weight, not diabetic, normal BP – in other words, pretty healthy. Thank you for your time and consideration!
Hello Jane Marie,
“Minimally invasive surgery” is a difficult-to-define and loaded term. The definition for what constitutes a “minimally invasive surgery” is not even agreed upon by surgeons. Everyone who requires a surgery wants that surgery to be minimally invasive. Does one incision accomplish a surgery less invasively than two or three incisions? An excellent surgical experience with a fast recovery and successful outcome depends on so many important variables, especially how gently the tissues are handled.
Many surgeons advertise that their techniques are minimally invasive to market their practices. I fully understand this. There has been a tremendous amount of pressure exerted by the general public and media, stressing the “little incision” and “minimally invasive techniques.” This also has produced a lot of compromised results.
In my practice, I emphasis absolutely precise implant positioning and soft tissue balance because this consistently produces the best results that last the longest. The surgery needs to be accomplished through the smallest incision with the least and gentlest soft tissue dissection and I emphasize meticulous soft tissue handling and closure. Buyer beware, I recommend you choose your surgeon and not the approach or prosthesis.
With regard to your second comment, if imaging studies (plain X-rays or MRIs) demonstrated arthritis with joint space narrowing, then I would not expect your symptoms to be improved with an arthroscopy. I suspect the goal of the anterior injection recommended by your doctor will be to place a local anesthetic and possibly a steroid into the joint. If, even temporarily, the pain is relieved and function and motion are improved because it no longer hurts, then that would be good evidence that you are being disabled from the arthritis in the joint and a THR might be a very reasonable and appropriate next step.
I hope this helps.
All the best,
Dr. William Leone
I am 34 and recently diagnosed with FAI and mild to moderate arthritis as a result. My doctor has mentioned the possibility of a THR instead of an arthroscopy. I feel that is premature. There is a chance that the surgery could make my hip arthritis worse but I don’t want to reduce my activity to the level a THR would. I think that if the mechanical abnormalities in my acetabular and femour are corrected I should have at least a a chance right?
Dear Rachid,
I appreciate and respect your desire to avoid THR. I also understand why your doctor has not encouraged a hip arthroscopy. If you have already developed mild to moderate hip arthritis, in my experience the likelihood of you having a satisfactory result with an arthroscopic surgery is very small and any early positive result from the procedure would be short-lived. Many times, the physical act of doing the arthroscopic surgery unintentionally imparts additional trauma to the articular surface (cartilage) and the arthritic condition worsens.
I would recommend avoiding THR as long as it’s “reasonable.” When you have reached that point when proceeding with THR is your only “reasonable” option, go into it with your eyes open. Discuss your hopes and expectations with your surgeon. Meet or talk with other people with whom you can relate and who have had their hips replaced. Try to learn as much as you can. I find a well-informed patient gets well faster and has a better, more realistic experience.
The limits you’ll want to impose on yourself after the procedure should be with the strategy of extending the prosthetic hip’s longevity. Individuals who have THRs can remain super active and athletic. Many people who have their hips replaced tell me that they “forget” that the hip is a prosthetic, so your brain and good judgment need to prevail.
I wish you only the best,
Dr. William Leone
I have an anterior labral tear (diagnosed by MRI) and mild arthritis. Constant worsening pain. Is a hip arthroscopy likely to be successful to remove the catching pain from the labral tear? I am 60 years old
thank you for your advice
Dear Debra,
Most likely you are going to benefit from a THR without first undergoing an arthroscopy. An arthroscopy may give you temporary relief if the symptoms are mechanical (i.e., locking, catching, giving way, or episodic) and are truly being caused from the torn labrum. You describe a “constant” worsening pain, which to me indicates it’s probably from the arthritic condition and not primarily the tear. Many, if not most, arthritic hips have secondary labral pathology. Also, in my experience, arthroscopy is rarely successful in 60-year-old patients with underlying arthritis.
I wish you the very best,
Dr. William Leone
I am a 45 years old very active woman. I have experience deep groin pain, weakness, also hamstring numbing pain. My Dr. (after contrast MRI and xray) told me I have a somewhat shallow socket and a labrum tear with some bone brusing. Also, no apparent damage in the cartilage He recommended a arthroscopy. At my age and given the diagnosis, will the procedure be effective? After reading many comment and reviews about this procedure I am nervous about going through it and the possible side effects. However I am not able to have a normal level of activity. I have been on modify level of activity and some PT for almost 5 months now, and no improvement. Thanks in advance for you reply.
Dear Erika,
From your description it sounds like you have a dysplastic hip with labral pathology. This is a very common etiology of hip arthritis and even more prevalent in women. The labral structure often is enlarged or hypertrophied in this condition rendering it vulnerable to tearing or separating from its attachment to the rim of the boney socket. Hyaline cartilage at this point of attachment often is injured also and lifts off the underlying supportive subchondral bone. This results in a chondral flap tear and sets the stage for osteoarthritis. If your symptoms are truly from the labral pathology, possibly an arthroscopy will relieve them at least temporarily. To truly correct the condition, the boney coverage of the ball must be improved as well as the labrum repaired. This is called a periacetabular osteotomy. It is a complex and difficult procedure which is not done frequently in this country. Usually it is reserved for patients in their teens, 20s or 30s. Of course, there are always exceptions. I’m concerned that you report that you have bone bruising. This is an MRI diagnosis, which describes bone edema and suggests localized abnormal stresses or trauma to the bone. I suspect it’s secondary to the abnormal forces being transmitted to an area of the acetabulum due to the lack of normal head coverage. It would also infer at least some degree of cartilage damage.
Ultimately, I think you’d benefit from a total hip replacement. I think an arthroscopy will have less chance of delivering the result you’re looking for. On the other hand, an arthroscopy will not burn any bridges and potentially might help, at least in the short run. I do hope these thoughts help.
I wish you the best,
Dr. William Leone
Hi Erika,
I am 43 years old. My name is Avesh Singh. You know at this age one would go for a hip scope rather than a hip replacement. It relieves the pain and pressure and with the meds somehow works in the long run. Leaving it will make it worse as you get older. Hope that help’s. Rgds Singh
I’m 57, have been diagnosed with a second hip labral tear (first one was scoped in 2007–and I had great results), and FAI in my right hip. I also have, apparently, too much arthritis for a hip arthroscopy but not enough for a total hip replacement. I recently had my 2nd ACL reconstruction in preparation for a left partial knee replacement (opposite side as my hip problems). I also have SI Joint dysfunction. I am clearly a Biomechanical mess from the waist down! I suspect I have a cartilage tear in my right knee, but I’m not telling anyone as it might delay any more necessary surgeries. My question is how much arthritis do I need to have before I can be considered for a total hip replacement? Or can I insist on a hip arthroscope to buy me some time? thanks.
Dear Betsy,
You very well may be a candidate for a total hip replacement if you are being disabled enough from the arthritic process in your hip. I wrote a recent article that describes exactly the situation you describe about yourself. That is, being advised that you would not be a candidate for another hip scope because of the extent of arthritis but that the arthritis is not severe enough for a replacement. If your symptoms are from the arthritis, then another hip arthroscopy will not help and very probably will accelerate the arthritic condition. If your symptoms are indeed from a torn labrum (i.e., symptoms that come and go, symptoms that seem mechanical, such as your hip locking) and you have significant articular cartilage loss, then still the chance of a scope giving you any lasting symptomatic relief is minimal and probably not worth the energy, expense and risks associated with repeat hip arthroscopy.
I suggest you discuss your concerns further with you doctor. Many patients’ symptoms and disabilities far exceed the appearance of their X-rays. Also, it’s been my experience that once someone’s hip becomes symptomatic from an arthritic process, the symptoms often progress much faster than that same patient’s knee symptoms.
The very best to you,
Dr. William Leone
dear dr leone,
I am very active 64 yr old; I have small posterior labral tear, moderate arthritis, and bone spur. my dr seems reluctant to do THR and recommended I see his associate for possible labral debridement. Isn’t that just a temporary fix for my condition?
Hello Steve,
In my opinion, having moderate degenerative arthritis and reactive changes (your bone spur) does not make you a good candidate for hip arthroscopy. Any benefit you might derive from the arthroscopy would be temporary and quite possibly the arthritic condition and your symptoms will worsen after. In my experience, 64-year-old, active men who have symptomatic arthritis do poorly after arthroscopy. Many are excellent candidates for total hip replacement.
I wish you the best.
Dr. William Leone
I am 43 years old and have had hip pain since I was working full time as a RN and pregnant with twins in my late 20’s. I was diagnosed with trochanter bursitis and had multiple injections and therapy and finally I had a bursa removed with a Z-tracking my IT band in 2008. It got some relief, but not for long. Recently my last 2 MRI’s have shown bone edema in the neck of my femur along with a small tear in the anterior labrum. The initial doctor who ordered the MRI called me and told me I had a stress fracture (he since retired and the new doctor I’ve seen does not acknowledge that finding).
My doctor even with these findings now wants me to get a back MRI (I have osteoarthritis with some narrowing in disc space L5-S1). Yes I have back pain and have had many injections in my back on the same side my hip hurts, but I think that has a lot to do with me limping for the last 15+ years. 99% of my pain is directly over the trochanter into the groin and down the front of my thigh with and without “catching”.
I have become a prisoner of my hip pain and my life has been greatly restricted because of it. I was an athlete most of my life and I have a long history of orthopedic injuries and surgeries (on other joints-13 surgeries total so far) as well as a huge family hx of osteoarthritis and joint replacements. I want to have it scoped so we at least know what exactly is going on, but my doctor is reluctant because of my age. I don’t want to wait for my hip to break or until I can’t walk at all before dealing with it. Am I wrong for wanting to have it scoped?
Thank you.
Dear Debbie,
I would consider having an intra-articular injection of a local anesthetic into your hip joint as a test. The physician who performs the injection might also want to add a steroid with the hope that it gives you longer-lasting relief. The injection would be a test, not a cure. If it does relieve your pain, it would strongly indicate that the pain is originating from your hip joint. Often, trochanter bursitis is a secondary symptom of an intra-articular problem, such as osteoarthritis.
Back pathology potentially can cause these same symptoms. I understand your physician’s concern that your symptoms might be originating from your back. An epidural injection could give insight as to whether your back is the real culprit. After bathing your nerve roots with a local anesthetic and steroid – at the level of your lumbar spine that forms the nerves that innervate your hip and greater trochanteric region – results in pain relief, then back etiology must be considered.
A hip arthroscopy is not a simple, benign procedure. I would hesitate to have an arthroscopy without a more specific understanding of the diagnosis and if it’s related to your symptom complex. Osteoarthritis does have a familial tendency and that very well may be the underlying problem.
I do wish you the best in your efforts to solve this problem and feel better.
Sincerely,
Dr. William Leone
Hi,
I am a 29 year old male and I was diagnosed with a labrum tear about 2 years ago. I actually tore it probably 4 years ago, but was misdiagnosed with a pulled groin(adductor) at first.
I had initially quit playing intense sports at first because of the developing groin pain from the labral tear. But over the last year, year and a half i have been starting to play more and more. I actually had a Synvisc one injection into my hip last year and that mixed with physiotherapy had actually helped a lot and was mostly pain free and started playing sports a little bit more again.
Recently i started playing soccer again but the hip just doesn’t feel right. It is not a really major pain, maybe slight pain or sometimes just nagging sensation. But it doesn’t last and then I am able to play again. I am just worried that the major pain may come back again.
My hip surgeon who recommended that Synvisc injection told me last year that because the tear is only a couple milometers, that it is not worth the risk of getting it scoped. That the surgery may lead to worse complications.
What are your thoughts?
Much appreciated.
Thanks
Dear Marc,
If your symptoms are truly from the labral tear and you have normal hip anatomy, then an arthroscopy might help you. If the labral tear is secondary to underlying arthritis or abnormal hip anatomy, such as dysplasia, any positive long-term results achieved with a scope may be disappointing. It’s been my experience with arthroscopy that results tend to be better if the scope is done sooner rather than later. I think your surgeon gave you good advice in suggesting that the benefits of an arthroscopy may not outweigh the risks.
The fact that you got symptomatic relief from the Synvisc injection suggests that your symptoms may be from joint arthritis and not the labrum. Many times, symptomatic labral tears create episodic and mechanical symptoms, such as catching, locking, giving way, pain with specific hip positions or a sense of instability. I would not expect you to have any significant relief with the Synvisc injection if your symptoms were from a torn labrum.
My advice would be to back off soccer and focus on activities that don’t cause pain, while keeping the muscles that control your hip really strong. You’re only 29 years old and you want to take care of your hips for the years to come. You don’t want to push yourself toward hip arthritis, or accelerate any arthritis that already has begun, or to the point of needing a total hip replacement, if you can avoid it.
I wish you the best,
Dr. William Leone
hi there,
I tore my ligament and cartilage in both hips from water skiing 2.5 years ago. I have had 3 hip scopes on one hip and two on the other. The left hip was due to the surgeon not removing enough bone for impingement. I am 3 weeks post op for the last cam shaving so we shall see if this works this time.
My right hip i had the first scope but unfortunately developed scar tissue, had another scope to remove it and now it has developed again. I am waiting for a 3rd on my right to remove scar tissue.
At what point do you advise to get a hip replacement vs more scopes? I do not yet have arthritis but i am in a large degree of pain.
Also with regards to scar tissue formation – how can you prevent that from occurring again?
Thanks
Hello Roz,
I expect that you’ll benefit from total hip replacement at some point in the future. I am concerned that ultimately you may not achieve the goal of pain free hips and the ability to resume an active lifestyle until total hips are done. I’m less optimistic that this goal will be achieved with hip arthroscopic surgery, especially considering the underlying anatomic abnormality that almost certainly has contributed to your problem. Also, although arthroscopic surgery can very effectively treat some specific pathologies, invariably some unintentional trauma also occurs to the hip joint cartilage. The more arthroscopic procedures performed, the more occurrence of unintentional trauma to cartilage.
My advice would be to fully rehab your hips after your recent surgery. If at that point you remain significantly disabled with pain and activity limitations, I would consider THR. I wish you all the best.
Sincerely,
Dr. William Leone
Sorry i forgot to mention I am mildy to moderately dysplastic which is another reason the scopes may not be working.
I am 36 and want to have kids in the next few years so PAO is out of the question.
Thank you
Hello Dr. Leon,
In the last few months I have done so much reading and research on the hip labral tear that I know more than I ever wanted to. I am glad to see your realistic and professional article on the arthroscopic surgery to correct this issue. Wondering if I can please get your opinion, as I have seen 3 doctors thus far and all gave me different answers. Maybe, definite no and definite yes…..
I just turned 40 and am VERY active (workout 6-7 days a week, tennis, weight lifting, swimming, hiking, HIIT/RIPPED classes, etc.). In 2003 I was in a bad car accident and my left side has not been the same since. Did get my 1st cordizone shot into my left hip then as was very painful and leaking fluid according to doctors. Decade has come and gone and about 12 months ago I started to notice some tightness in the groin area, some instability and mainly issues with bringing the knee to the abdomen. In kickboxing classes the motion was starting to be problematic and now at the point I had to stop taking them as cannot really bring my left leg that high. My hip snaps at night or if swing the leg in certain degree, etc. At first I was misdiagnosed in Oct last year as thought tight SOAs muscles ad after 5 weeks in PT it was getting worse so I requested MRI in Dec 2014, which showed 1.5cm tear as well as some signs of arthritis and some fluid present. I did get cordizone shot that helped but by now wore off.
To add to this my left leg is 3/4 inch shorter than my right and I have bad scolisosis as well- have been dealing with back issues on and off since my car accident especially but scoliosis and leg has been with me since childhood.
As I have mentioned- three different opinions from three different doctors and the more I read the less success ratio plus lengthy recovery. Frankly I am wondering since I can still play tennis at 70%, walk, hike on moderate trails though I have to alter swimming, classes, etc.- am I the right person to get into this surgery or should I just carry on until I get THR say 10-15 years from now?
Lastly, if I do NOT have the surgery- can the tear get larger or assuming it happened with the car crash and impact, it will stay the same? Is the arthritis going to get worse? Can surgery add to the arthritis getting worse?
Dear Gabriela,
I would not expect you to get significant long-term relief or a “cure” from a hip arthroscopy. I suspect your arthritis is secondary to the trauma the joint sustained from the car accident so many years ago, but cannot say for sure. Is there also some degree of hip dysplasia or some other abnormality possibly related to your scoliosis? Have you developed similar, though subtler symptoms on the other side? Your labral tear might be due to new trauma from all of your activities or may be secondary to the underlying arthritic condition. Regardless, in general hip arthroscopy patients do not do well when there is underlying arthritis. If a scope is done, it also is common for the arthritic condition to worsen.
I think at some point total hip replacement would be a tremendous help to you. I would try to delay having that surgery as long as you reasonably can. I would recommend developing a personal strategy to avoid those activities that are aggravating your hip condition as they are hastening your hip’s demise. At some point, if you do proceed to hip replacement, you’ll still want to employ this strategy to care for your new joint. I would avoid kickboxing and other extreme impact activities now and after hip replacement.
The best of luck to you,
Dr. William Leone
Hello Dr. Leone,
I am 44, was very active up until this early winter, due to hip pain since last summer that led me to seek out MD care. My sypmtoms came on gradually since last summer when I did an easy re-entry into running, from a ten-yr hiatus. First just tightness at the ASIS, then after months of still running, thinking it’d go away, the discomfort became more global and diffuse. Xray doesn’t point to any significant findings, but MRI does show a high grade loss of cartilage (1cm? according to MD), and the MD thinking is that it is from an injury. I have no recollection of any injury to my hip, except about 5 months ago during a yoga move (internal rot). Right afterward, I was unable to bear weight through the limb, but after a bit was able to again and carried on into my day (labral tear? Cartilage damage then?). My PT and MD prior to the MRI were suspicious of a labral tear from early on. Nothing showed on MRI. Is it possible that the MRI arthrogram missed the tear (other plane not captured by MRI?), and that this is the cause of my symptoms? Is it possible I could have had the chondrolysis for years and be asymptomatic? Would a physician scope my hip to look for a labral tear? I am not so keen on going for the micro fracture procedure, but I would be interested in finding out if I do indeed have an undiagnosed labral tear.
Hello Joanne,
Most likely your symptoms are from osteoarthritis. I wonder if your hip joint anatomy is normal and if there is some underlying reason why you would develop an area of full-thickness cartilage loss. The location of the cartilage loss may also give a clue regarding its etiology.
If you have hip dysplasia (on the x-ray, it looks like the femoral head is not fully covered by the socket or acetabulum) and a torn labrum, then hip arthroscopy won’t lead to a good result and I wouldn’t recommend it.
It is possible the MRI did not pick up on the tear. All MRIs are not the same quality. I would not recommend having an arthroscopy primarily to look for a tear. I don’t think the benefits would outweigh the risks. If a decision is made to attempt to treat the arthritic area with microfracture or another joint preservation technique, and labral pathology is discovered, it can be addressed at that time.
Conservatively, I would avoid those positions and activities that exacerbate the discomfort and accelerate the degenerative process.
I have linked back below a previous blog post that might be of more help.
http://holycrossleonecenter.com/blog/joint-preservation-strategies-delay-need-hip-knee-replacement-surgery/
Best of luck to you,
Dr. William Leone
Hi! This is a very good article with great information! I think I have read everything I can possibly find online about THR vs arthroscopic surgery!
I am a 33 yr old that has been suffering from hip pain since I was a teenager. I am also an RA patient. I began having irretractable pain about 10 months ago when I went to my PCP and had a hip xray that showed abnormal findings and was referred to an arthroscopic hip specialist. He performed a different set of xrays that revealed a possible abnormality in the femoral head. His indication was a probable labral tear. Well…. MRI results revealed much more
” at the 2:00 to 1:00 position of the anterior superior right hip labrum there is an intermediate grade partial thickness under surface tear of the mid substance of the labrum. This involves approximately 50% of expected labral thickness. Additional free edge truncation noted throughout the anterior superior labrum. At the anterior superior aspect of the right accetabelum there is a 12 mm AP by 6 mm transverse focus of subchondral cystic change indicating occult overlying grade 4 chondral loss. Additional areas of grade 2 and 3 chondral thinning noted of the superior aspects of the right hip joint. No significant cortical remodeling identified.
At the superior margin of the femoral head neck junction there is a tiny cam lesion.
Mild public osteoarthritis noted.
There is also subchondral cystic change associated with the grade 4 chondral loss.
The arthroscopic surgeon will not operate in me with the degree of damage I have done in my joint. I received an injection which provided some relief for About a week.
I was referred to an ortho. That specializes in knee and hip replacements only. He also agreed that arthroscopic surgery would probably not benefit me. I am scheduled for a hip replacement on July 6th. In the meantime I went to see a new rheumatologist. He performed his own xrays and says he doesn’t see anything on my xrays…. long story short, he wants me to go get a 3rd opinion and try arthroscopic surgery 1st. My issue with that is I am really tired of bandaids. My age has been brought up with both surgeons as these are not normal findings on a 33 yr old. Yet if I was 50 there would be no questions about the fact that I need a hip replacement. I am tired of living in pain, I can’t walk for much of a distance, I can’t sleep, hurts to drive, and I have 2 young children that I feel like I am missing out on! I am ready for this surgery and the surgeon even this that the implant he is going to use can last the rest of my life! I am now confused on what to do.
What are your thoughts based on these findings?
Thank you so much for your time!
Heather Morgan
Dear Heather,
I agree with the opinions you’ve received from the arthroscopic surgeon and joint-replacement surgeon. I, too, do not believe you will get any meaningful relief from an arthroscopy. Fortunately, the pathology described can be treated very effectively and predictably with a total hip replacement. The longevity our hip implants has never been better. I understand your frustration and need to become active again, especially with your kids.
I wish you only the very best,
Dr. William Leone
Hi, thank you for this article.
I am an active 32 year old woman and was diagnosed with idiopathic transient osteoporosis four months ago. At the time I was told to stay away from impact exercise and wait for the osteoporosis to resolve itself. Bloodwork ruled out autoimmune/metabolic conditions and a DEXA scan showed my bone density to be normal overall. In other words it was just my right femur that was affected by the patchy osteoporosis.
The symptoms started in December of 2014 and I only got the MRI and osteoporosis diagnosis in March after physiotherapy failed to improve symptoms. In June I started having less pain. My doctor, who had put me on fosavance (a bisphosphinate) for the osteoporosis in March ordered an MRI in June to see if the medication had improved matters. Despite having less pain now the MRI showed a tension side stress fracture of the femoral neck, both March and June MRIs showed evidence of labral degeneration. 5 different orthos have recommended that I get screws put into my hip to prevent displacement. One ortho has also recommended hip arthroscopy (while I’m under for the screws) to treat labral degeneration. He has used stem cells in the past and recommends this for both the fracture site and the labrum if need be (to be determined after insertion of the scope). I went back to the initial ortho and he said this was an overly aggressive approach, that all I need are the screws and that the rest (harvesting cells from marrow further down in my femur, hip arthroscopy) sound overly traumatic. I’m left feeling a confused and would be very grateful for your thoughts.
Thank you and best wishes!
Mona
Dear Mona,
I also agree with your original orthopedic surgeon. I think having two hip screws placed into your femoral neck and head and across the fracture (with the hope of preventing the femoral neck fracture from displacing) to promote healing is appropriate. I would discourage specific treatment for the labral tear at this time. Many folks have labral tears that are asymptomatic. They don’t even know their labrum is torn because they’ve never gotten a MRI.
An arthroscopic hip procedure is not a simple, easy, atraumatic operation or rehabilitation and I would be especially hesitant to recommend having your hip scoped at this time, considering the weakened state of your bones from the transient osteoporosis further complicated with your femoral neck fracture. In my opinion your main priority should be to do everything you can to assure that the hip fracture does not displace and ultimately heals. If this happens, it will preserve your own hip and prevent a whole host of potential problems. If in the future you find that you are symptomatic from labral pathology not the hip fracture, and your bone density has recovered, then I would consider a scope.
I wish you the very best.
Dr. William Leone
I am a 57yr old woman. I have osteopenia and bi lateral hip pain, I was told I have osteoarthritis in my hips. I am having pain walking, getting in and out of cars. Leg and thigh pain when being intimate, are there any none invasive procedure that I may be a candidate for. And what is the down time, I am still trying to work, however it’s difficult.
Dear Sharon,
A total hip replacement (THR) should be considered only after you have exhausted all the nonsurgical or conservative measures that can minimize symptoms and allow you to life fully for as long as possible. It becomes appropriate to capitulate when conservative measures no longer control the pain and you feel limited from living a full and active life. I will refer you to a blog article I wrote describing these conservative measures.
That said, from how you describe you present state, it sounds like you would be greatly helped with by having THR. I think what has changed the most during my 25 years of practicing orthopedics and specializing in this specific area is how much faster patients on average recovery as compared to even a few years ago. Again, I have linked above to a blog I wrote describing the reasons.
Most of my 57-year-old patients get out of bed the day of surgery and walk, and then go home the next day to continue therapy. Most shower four days post-op and begin diving approximately two weeks after surgery. I also encourage patients to begin exercising in a pool. Depending on what a patient’s job is and the motivation to get back to work, someone can return anywhere after one to three weeks. The motivation and need to get back to work is a huge factor here.
I wish you all the best,
Dr. William Leone
I am a 37 year old and have been diagnosed with a torn labrum, CAM impingement, para acetabular cyst and minimal arthritis. In the past my hip has hurt and had mild-moderate catching sensation. Recently it has become fairly asymptomatic with intermittent periods of pain. I am extremely active and want to stay that way. Would I be a good candidate for arthroscopic surgery to preserve the joint? I get the impression it’s not bad enough for a THA but may only degenerate with time and activity.
Any thoughts would be appreciated.
Thanks,
Jon W.
Dear Jon,
You probably are not a great candidate for hip arthroscopy, however I would suggest being evaluated by an orthopedic surgeon who does arthroscopy, specifically for his or her insight. I think at age 37, every attempt should be made to preserve the joint and delay joint replacement if possible.
The fact that your symptoms are intermittent suggests that possibly a limited arthroscopy could address the intra-articular pathology which is causing these mechanical symptoms such as an unstable flap of a torn labrum. That being said, you don’t want to have a hip arthroscopy if you’re not going to do well.
I wish you the best,
Dr. William Leone
Hi,
I am an active 28 year old with a labral tear in my left hip. The pain has been on the outside of the left hip for the past 3 months and the MRI shows a labral tear. I have gone to PT for the last 6 weeks and the pain is not going away. I got a cortisone shot and it only helped for about a week and now the pain is back. The x-rays show that I have normal hip structure so the doctor recommended hip arthroscopy to repair the tear. The pain is pretty consistently there and gets worse after walking a lot or going to PT. Do you think moving forward with the surgery is the right decision?
Thanks,
Michelle
Dear Michelle,
From the description you provided including temporary pain relief with a cortisone injection, failure with PT, a normal hip X-ray with normal morphology, and symptoms that are not resolving with time, it sounds like you would be a very good candidate for a hip arthroscopy.
The best of luck,
Dr. William Leone
Dear Dr. Leone,
I am a very active 57 year old . I am a runner, a tennis player and a person who must move as much as breathe. I have been diagnosed through an MRI with tear of the labrum. There are no significant degenerative changes, no fractures, no regions of bone destruction. I want to remain active and would like to think that I could return to The activities that i enjoy.An arthroscopic repair if the labrum has been recommended. Your thoughts?
Dear Ann,
From how you describe your condition, you very well may be an excellent candidate for hip arthroscopy.
I wish you the very best,
Dr. William Leone
Hi,
I’m 41 years old male that injured my hip a year ago playing sports. At first I thought it was a groin pull, but the pain didn’t go away for the full month I stayed off it with no sports/exercise. The X-rays revealed no FAI or arthritis. The first orthopedic doctor I went to offered to give me a cortisone injection or I could get an MRI to see what the problem was…I opted for the MRI because I didn’t want to degrade the joint with the shot. The MRI came back as a “partial labral tear of the left hip” and he offered to do the surgery.
I got another opinion because he didn’t specialize in the surgery. The second doctor had a x-ray guided hip injection ordered which stopped the pain for several days. Because of the relief in pain he said he would do the surgery. At this time (5 months after the injury) I opted to put the surgery off because the pain was now minimal and would only come back when I ran or made side-to-side movements. It is now August and I thought I would do the surgery and use the winter months to recover because I ‘m a very active person and wanted to get back to sports.
Any thoughts you have would be appreciated
Thank you,
Chad
Dear Chad,
The fact that you did get significant though temporary relief after an intra-articular cortisone injection strongly supports that the hip symptoms are being caused by a hip intra-articular problem. Your description that symptoms are caused with running or lateral movements also could support a diagnosis of unstable labral tear. If this is the etiology of your symptoms, then arthroscopic surgery could possibly provide relief. It’s been my experience that when an arthroscopy is done closer to start of an injury, rather than later, then results tend to be more predictable. Other injuries can occur as a result of the labral tear, such as cartilage delamination which can lead to arthritis. It’s my opinion that if you are going to have a scope, the sooner the better. Having a scope is not a sure thing. Often more pathology than just the labral tear is discovered and even in the best of hands, some degree of chondral injury is inevitable.
My recommendation is to discuss it further with you doctor and ask his or her opinion. I would also ask yourself if you’re truly “disabled” enough.
I wish you the best,
Dr. William Leone
Hello Dr. Leone,
I am a 33 year old male and I used to be fairly active. My deep groin ache started about a year ago without an acute injury or episode. It just kind of came on one day combined with some muscle aches in the oblique area on my right side. I had mesh hernia surgery but that did not resolve the deep ache in the crease/groin area. I have tried a few injections, acupuncture, massage therapy, chiropractors, physical therapy, stretching, home programs to strengthen the surrounding muscles and I have had little progress. All MRIs on spine were clear. X-rays confirmed by 3 hip specialists show confirmed FAI in their eyes. MR Arthrogram w Contrast did not reveal anything concrete but my hip surgeon gives an 80% chance the Arthroscopy will fix me. The injections did nothing and we have not been able to reproduce the deep, stabbing pain in the groin I have felt 2-3 times over the past year. I haven’t tried running (I am not a runner). The pain comes about in my groin and oblique area after prolonged sitting in cars or planes. Its just an intermittent deep dull ache on the right groin side. My left adductor is now out of wack these past 6 months but overall the pain is manageable but annoying. I have not really pushed myself too much in fear of making it worse. It definitely has effected my life and lifestyle the past 14 months. I want to get back to working out and being able to sit in my car or through a movie. My surgeon, who does over 200 hip arthroscopies a year and is very experienced, thinks I should have the surgery and it is scheduled for next week. What is your opinion on if I should go through with it? I just need a change…this deep dull ache cannot be a muscle problem as I have done everything under the sun to try and resolve it. Thanks!
Dear Arthur,
It sounds like you’re not happy with your present limitations and the symptoms are not resolving on their own. Three orthopedists have confirmed FAI and you’ve found a very experienced hip arthroscopist who feels confident that he can “fix” your hip. If you have a hip arthroscopy and do well, it will give you a chance of relieving your discomfort and hopefully protect the joint from the consequences of the FAI leading to arthritis in the future. If you do poorly, you will not have “burned the bridge” to have a hip replacement.
I wish you well.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone,
I’m 23 years old – I have hip dysplasia & have had since I was born. I have no tears, I have bone on bone contact between my ball and socket. When I was 19 it got so bad I had to go and do physio & take pain relief, now however it has gotten worse, the physio or pain relief do nothing. I have been told to consider hip arthroscope as I’m only young however I have also been told to consider a hip replacement. The pain is unbearable and I don’t take kindly to many medications. I am unsure which to go with & would like to know what you think.
Regards,
Kelly.
Dear Kelly,
If you have developed “bone-on-bone contact,” then you almost certainly are not a good candidate for a hip arthroscopy. Further, a hip scope will not treat the underlying abnormal hip mechanics caused by the dysplasia that lead to your arthritis. Truly, if you have extinguished the full list of conservative measures including weight loss, muscles strengthening and conditioning, and still no longer feel you can live with the discomfort and limitations, then you may be a candidate for total hip replacement or periacetabular osteotomy (PAO). Each has advantages and disadvantages. My recommendation would be to learn as much about both treatments as possible, be evaluated by professionals who are experts in these areas and then make a decision based on your individual needs and desires.
I wish you well.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hi I am 41 years old. And I just had an arthroscopic labrum tear hip surgery three weeks ag.
But, I am still having the same popping and snatching in my hip.
The pain can be unbearable especially in my groin area and butt cheak.
And I have lost my appetite. My mouth and throat is always dry.
Right after surgery I also started getting blisters inside my mouth and tongue. And blisters on the corners of my lips.
I also have to start baring weight on my hip. But I can barely stand the pain. But I am not giving up nor will I push myself to far.
Seems like the pain is at the same level before the surgery. I have a slipped disc and a bulgingdisc in ba. One disc is stastarting to deteriate. I don’t know what to do with everything. I have been out of work since February.
Dear Margaret,
It is a concern that you report having the same pain and mechanical symptoms now that you were experiencing prior to your surgery. I would recommend you return to your surgeon for further evaluation.
Typically, patients are dosed with an IV antibiotic just prior to hip surgery and over the first 24 hours after surgery. Occasionally, patients develop oral thrush (a mouth fungal infection) after treatment with antibiotics due to disruption of their normal bacterial flora. Antibiotics can cause other unintended reactions and problems as well. Further, the stress of surgery and continued pain also can exacerbate a viral infection such as herpes. I also would encourage you to see you primary care physician so he or she can examine you and make recommendations as well.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello,
I am a 28 year old female (5’2″ 135lbs). I am an athletic female. About 8 months ago I began having pain in the front of my left hip that I would especially feel when I would back squat with a heavy weight on my back. It would feel like pinching. At first I would just work through the pain and continue to squat with heavy weight and continue with olympic lifting. However, the pain continued and my squat numbers started to drop even though my training was not only different. Due to this I thought some physical therapy, which also didn’t help. So I finally got an MRI. MRI revealed that I have an anterior/superior labral tear of my left hip. It involves the labral body and its attachment to the acetabulum. The MRI states that there is no fracture or dislocation, no hip dysplasia, no evidence of femoral acetabular impingement, no abnormal acetabular version. Articular cartilage is preserved. Hip capsule and soft tissue are normal. I don’t have a lot of pain with this…the hip starts to ache after prolonged sitting, I have some popping/clicking at times, but the only time I feel real pain is if I try to squat with heavy weight (going below parallel). I don’t think physical therapy will be much help for me as I am an athlete and my hips are strong. I have stopped all squatting and olympic lifting for the past couple of months. The pain is the same. My goal is to be able to squat 240 lbs again and be able to go back to olympic lifting without any pain or weakness in my hip. With the result of my MRI and my goals…would I be a good candidate for hip arthroscopy to fix the labral tear? My only fear is that the surgery will not produce the results I want and potentially cause more pain/problems.
Dear Ksenia,
From what you describe, you would be an excellent candidate for hip arthroscopy with the goal of curing your present symptoms and preserving your hip function for years to come. Many times, a torn labrum is the precursor for degenerative arthritis. I think the goal of having hip arthroscopy should be to relieve your discomfort by reconstructing your hip anatomy as close to normal as possible with the hope of staving off hip problems in the future. I would not recommend that you resume heavy weight lifting with your legs after having your labrum repaired. Whatever mechanism injured you hip the first time very likely would do it again. I truly think this would be self-destructive behavior.
All the best
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hi Dr. Leone,
I am an active 54-year-old women, diagnosed with mild arthritis in both hips and a labral tear on the left. I have had cortisone which took care of most of the pain but I still get bouts of catching and ‘take my breath away’ bouts of pain on the left only. I can’t walk great distances or play tennis anymore. I do ride a stationary bike and swim with mild pain on my left side only. I think that an arthroscopy will help on my left side because I have arthritis on my right side but it doesn’t hurt, and I think it’s because of the torn labrum on the left. What do you think? I’d like to push off the THR if I can by seeing what kind of results I get from the arthroscopy.
Dear Dr. Leone,
I am a 56 year old female and have had intermittent left hip pain for about 26 years since my first pregnancy. It was mis-diagnosed as various other things through the years, and has become more frequently bothersome in the past few years. I underwent a MRA with contrast which showed: a tear of the anterior acetabular labrum, chondral delamination of the adjacent acetabulum, subcortical cyst formation, sclerosis and bone marrow edema, large subcortical cysts of the anterior superior femoral head, a pistol grip deformity of osteophytes, a cam type dysplastic bump, and synovitis. From reading your responses I am thinking that a hip arthroscopy would not be effective and that maybe I should just hold out and wait to have a THR. Would you agree, or do you think I would benefit from an arthroscopy? I am not debilitated yet, and can do fairly normal daily activities, but my hip catches frequently when I turn or twist and I feel falling could be possible. Any insight you could give would be appreciated. Thank you!
Dear Suzy,
I do not think an arthroscopy would help you. It sounds like at some point, a total hip replacement would be life changing for you. I would delay THR until your feel in your heat that “you are ready.” This decision is different for everyone. The timing would probably be right for you when you are closer to feeling “debilitated” or limited, or you are feeling so vulnerable and frustrated that cannot see any other way.
I wish you only the best.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Terri,
Most arthritic hips that I operate on also have secondary labral pathology. If you have arthritis in both hips, then I don’t think your going to realize any significant benefit from having a hip arthroscopy. Fortunately, the condition you do describe is exactly the condition that THR can treat very predictably and effectively. I suspect at some point hip replacements will help you tremendously.
I wish you well.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello my name is Stuart and am a fitness instructor and competitive athlete.
Three years ago a developed a vague buttock/ proximal hamstring niggle. I cannot pin point why but I remember doing some deep heavy squats in training.
I was able to carry on with my racing but was aware of strange buttock feeling after a few miles. I therefore went for a xray but it showed nothing. I then had PT but nothing changed. I had an mri but it showed nothing.
Then my niggle became an injury after 12 months as I got a clicking with anterior and lateral hip pain, So I was given cortisone into glute medius. This gave me some relief and I was able to return to track racing. Then 5 months ago the clicking returned within hip extension stiffness at end range plus the return of pain at full flexion and full internal and external rotation. Therefore I had an MRA but it showed nothing. So I had a intra articular diagnostic injection with cortisone. I got relief from this for a while.
My surgeon says he will do hip a scope. I sure hope it works out as this is affected my family life and work.
Do you think I’m a good candidate, I’m now 39 years old?
Many thanks
Stuart
Dear Stuart,
I’m concerned that a definitive pathology has not been determined, even after having an MRI with arthrogram (MRA). I would consider having other surgeons and radiologists review the films both for diagnosis and to assess the quality of the study. The quality of the MRI scanner, as well as the specific software and sequences used, makes a huge difference in the quality of images and information gleaned. In general, performing an “exploratory” hip scope without going in with a specific diagnosis and plan is not a high-percentage operation. Hip arthroscopy is not a benign procedure and symptoms occasionally do worsen after the procedure. Risks must be weighed against benefits.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone,
Thank you for all this information.
I’m 44 diagnosed with minimal labral tear and impingement in my left hip. I used to do yoga and taichi nearly on a daily basis (some of that may have caused the problem), but a year ago after having to cycle for a month things got worse, and since then I’ve been having pains in this joint. Stopping the yoga and taichi has actually helped and I’m now swimming mildly. This keeps me in shape. I have better days and worse days, but I don’t limp and I’m functioning well.
After consulting with an arthroscopy surgeon yesterday he said that this can certainly be operated, but also said that I can try physiotherapy (Mulligan technique?) and that some patients have actually avoided surgery this way.I understand that labral tears can be fixed only by surgery, but have you experienced people with this kind of condition that managed to illiminate the pain and return to full activity by physiotherapy or other alternatives? Or do you think I should just go ahead with the surgery? Will continuing this way eventually lead to a surgery anyhow?
Many thanks,
Oren
Dear Oren,
I think it’s always reasonable, if possible, to try and resolve any condition with methods other than surgery. A trial period with good physical therapy certainly is reasonable. If your symptoms are mechanical in nature from an unstable labrial tear, I suspect that in the long run you’ll still request surgery to hopefully solve the problem. If in you heart you know that you ultimately are going to request surgery, I would recommend doing it sooner rather than later because I think the results are more predictable when done early on and there will be less chance of secondary hip arthritis.
I wish you a full and satisfactory recovery.
Sincerely,
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone,
Im a 23 year old male and was recommended a hip arthroscopy surgery. I used to play football a lot and had an injury around the groin area more than a year ago. I have developed ossification that can be seen on my right hip with x-rays and MRI (I don’t know if this is related to my groin injury). I was diagnosed and my doctor gave me the following options:
1. Do nothing.
2. Injection therapy for symptom control only but it will be a temporary measure.
3. Hip arthroscopy for femoroacetabular impingement on the right side dealing with the
heterotrophic ossification arthroscopically where it is impinging anteriorly as well as undertaking intra articular structure repair using arthroscopy both addressing the acetabular labrum and if articular cartilage is involved then using bone marrow harvested mesenchymal stem cells (BMAC) in an attempt to regenerate the tissues. Overall the chances of success are in the region of 85% with 5% risk of worsening the matters. The rehab is going to be typically 3-4 months.
I have read about the hip arthroscopy surgery and I was worried about the implications that can occur from it. However, I feel pain in my hip and it is getting worse as time goes by. Would you be kind enough to share your views on the matter, and whether the risk of doing nothing outweighs that of doing the surgery. Much appreciated.
Dear Ibrahim,
Your physician’s approach outline sounds reasonable, especially considering that you are only 23 years old – if you feel disabled enough. That is a personal question that only you can answer. I don’t know if the given chance of success versus failure is actuate, but in general the bar is set lower when a patient is only 23 years old, factoring in more risk with surgery (higher risk of failure or worsening of the arthritic process) with the hope of stopping progressive demise, as well as relieving symptoms.
Recognize that the surgery is technically difficult. Often when heterotopic bone is present, it’s not actually causing symptoms or impingement. Resection is reasonable if intra-capsular (actually it would be imbedded in the hip joint capsule and most of the HO would be extra-articular in muscle) and causing symptoms and/or impingement. Heterotopic bone may also reoccur after surgery due to the trauma caused by the surgery and your genetic predisposition which lead to its development in the first place.
If your heterotopic ossification is extensive and truly inhibiting your range of motion, then I should think an open debridement would be more satisfactory coupled with preoperative or postoperative low dose radiation in the hope of preventing or minimizing its redevelopment.
I wish you luck and a full recovery.
Sincerely,
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone
I am a 41 year old male. My hip pain has become progressively worse over the last 18 months, and has now reached the point where I have stopped impact exercises and significantly reduced lifting heavy objects and walking moderate distances. I seldom if ever experience sharp pain, in most cases I suffer from dull aches at the end of the day with occasional tightness and soreness in my upper groin, and outer hip area. In some cases I have pain in my deep groin. I used to run moderate distances and was active in sport but have never experienced a hip injury.
Hip specialists have offered mixed opinions regarding my condition and course of treatment. X-rays indicate obvious bilateral pistol-grip deformities, but with good joint spacing. However there is also partial uncovering of the femoral head (Wibur angle approximately 24 degrees) indicating what looks like a mild dysplasia. MRI results also indicate good cartilage condition, with the exception of very small labral tears and some small cyst formation in both joints. No one has indicated arthritis. The clinical tests for indicating hip impingement t(inward rotation) caused me discomfort but not what I would describe as pain. And my hip range of motion is good, although at times I get discomfort leaning forward or sitting in a deep crouch.
At present there are differing views for how to proceed. One sports medicine specialist and hip specialist have recommended FAI surgery, and indicated that the femoral head uncovering is not a concern for them. However other hip specialists and a sports medicine specialist have concerns about my dysplasia and do not recommend any FAI or arthroscopy (and also note that my condition and age are such that a POA is not recommended). They have recommended conservative treatment such as physical therapy and modified activities, the goal of which is to delay a THR.
I would like to know whether or not I am a good candidate for FAI. Those recommending FAI have told told me my impingement is causing labral damage. Whereas those recommending waiting until THR, are concerned about any arthroscopic intervention whatsoever. My condition from imaging is indeed bilateral. However, my pain is noticeably worse on my left side, and my range of motion on my left side is slightly worse than the right.
I am also curious as to what could be causing my pain if indeed my X-rays show good joint spacing.
I am interested to know your viewpoint. Best regards.
Dear Jonah,
I think ultimately you are going to need THR surgeries. You should consider proceeding with these surgeries only when you feel your disability has become debilitating enough to you. This is personal decision and everyone has a different threshold and trigger.
Your hip condition is congenital. Your lack of full head coverage and impingement led to your labral and cartilage damage. The cysts you describe are consistent with this. Are these cyst extra articular or intra osseous (in the bone i.e., geods)?
PAO would address the abnormal mechanics and may delay THR. It’s a complex surgery that is not commonly done in this country and is associated with its own complications. Many would discourage it in a 41-year-old person. I think seeing an orthopedist who has expertise in PAO is reasonable, so you feel fully informed. An orthopedist experienced with PAO may have different views based on his/her personal experience and expertise.
Further, I suspect hip arthroscopy is not being fully endorsed because it will not address the biomechanical abnormality that underlies your problem (dysplasia), though it may give you some temporary relief. Typically, a significant rehab is associated with the procedure and, once again, it is not without complications. Many would not recommend arthroscopy if there is any underlying arthritis.
I think the conservative advice you received is spot on: activity modifications, physical therapy, and possibly an NSAID. Do your homework. Fortunately at some point, I believe someone will be able to help you definitively with THRs.
I wish you good health and a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone
Thanks for your prompt, professional reply. The cysts I reported are intraosseus and can only be seen clearly on a CAT scan.
Complicating matters for me is the fact that I am on an expat assignment in East Asia where the ability to visit American hospitals and clinics is limited. My job is not physically demanding which makes some things easier. That said the health care facility in my country has board certified American surgeons (and the British equivalent) without flying to the U.S. Both are recommending FAI impingement surgery. Interestingly, the British surgeon is a hip specialist who performs POA’s somewhat regularly (in addition to replacements/revisions). Until now, no one has the opinion that the degree of dysplasia warrants this very involved surgery at my age, but I like your idea of getting a second opinion from a dysplasia expert (POA surgeon) to if only to help me understand this specific condition, its severity, and what this will mean for me in the future.
Regarding my bilateral gunstock CAMS I have a small dilemma. The local surgeons are convinced that the cyst formation (and location) are resulting more (if not only) from the CAM impingement. They have warned me that I have a relatively short time window to act before irreversible arthritic damage being caused by the CAMs becomes so great that arthroscopy can no longer be regarded as an effective treatment. They believe that I will experience relief as soon as my FAI surgery is complete, and that my dysplasia is not present, or in the worst case “mild.” And that I should not wait too long.
But there are other opinions. The U.S. doctors believe arthroscopy can provide only short-lived relief from an inevitable problem, whereas others feel that arthroscopy and even accelerate dysplasia symptoms. One experienced U.S. sports medicine specialist (arthroscopy) has the same concern about dysplasia as what you reported.
On one hand the prospect of watching my hips slowly deteriorate is a little depressing. Accepting that the THR is the only solution is hard to take, especially considering that I have three young children whose physical interaction I try to balance against preserving my health, future revisions, etc. On the other hand, my situation could be worse and I am not in daily pain (I would say discomfort / fatigue). For reasons I do not understand, physical therapy seems to have helped me. I take OTC quantities of NSAID, and recently have been able to reduce my daily intake from the maximum 3 doses, to an average of 1-2 daily doses after therapy. I am now much stronger and much more flexible.
More than likely I will try to schedule appointments with one POA specialist and one additional sports-medicine Doctor during my next home leave in the summer. Really for the purpose of learning more. All of this said I am concerned about how quickly damage to the hips can manifest (compared to other joints). If THR is the only solution, I am willing to accept this and prepare myself accordingly. Everyone agrees that THR makes for a good outcome for most patients suffering from arthritis resulting from dysplasia. It is just that I grow frustrated when multiple professionals have not raised concerns about my dysplasia and are encouraging me to act with a different procedure and act soon!
I agree with you, if a THR is necessary anyway, why go through other procedures? But for better or worse, some doctors have presented FAI surgery as an alternative which will be effective as long as I act soon. Can this be correct? For peace of mind I want to reject or accept this assertion as soon as possible.
Thanks for your interest and professionalism
David (Jonah)
@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@
P.S. Is it possible that your moderator change my blog name to David. I have some concerns about my anonymity and those of my providers here.
Hi Doc , Let me start off saying I’m a 40 year old male that had hip dysplasia as a kid. Right hip I was in a body cast for three months. A year later the left hip went out and I had the surgery. Hip was pinned and I was on crutches for three months. Fast forward 30 years later and the pinned hip is bone on bone in two places. Doctor says I’m too young for THR , says I can do injections or arthroscopy . She says she don’t think the arthorscpry will work . What should I do?
Note* the hip was pinned to high caused the femoral head to rub the wrong way.
Dear Ed,
I think you are going to benefit from having a hip replacement at some point. The appropriate time will be when you feel miserable enough form the discomfort and compromises in your life that you see no other choice. That time may come sooner rather than later. Having a hip replacement as a young man is not optimal but almost certainly will be your reality. I don’t believe that an arthroscopy or repeated injections would be beneficial. It is critically important that your hip replacement is done well the first time.
I wish you well.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I am 42 year old female with a CAM impingement and a labral tear that I think happened in September 2015. I have been told that I am a good candidate for surgery to fix the impingement and tear as I have no signs of early arthritis in the hip.
One surgeon is a cartilage-preservation specialist and recommends a repair if PT does not manage symptoms (results mixed so far). Another is a strong proponent of labral reconstruction with donor tissue, and has impressive short-term results (low revision rates, happy patients) to back up his technique. However, since this is a newer procedure it is not fully covered by insurance and not validated by long term (15-20 year) longitudinal tracking, which gives me pause.
Is this split typical among hip arthroscopy specialists? Does the debate seem to be swinging in one way or the other? As a patient with (hopefully) many more years of skiing, hiking, volleyball and mountain biking ahead of me, this feels like a monumental decision.
Thank you for your interesting article and thoughtful responses in this thread!
Dear LK Mort,
It is a good sign that two hip arthroscopic specialists feel that they can help you with hip arthroscopy. You are insightful to recognize that different opinions exit regarding “the best” method and what we consider the best practice now almost certainly will change with time. I honestly don’t know which method has the best tract record and which will lead to the highest longevity. I would at least add to my calculus the increased risks associated with using cadaver tissue. While the risk of rejection and infection is very minimal, it is not zero.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
hi i was hoping you can give me some advice? for the last 2 years i have had x2 hip arthroscopys ( one in july 2014 and a repeat in april 2015) , including repairs and debridement of labral tears and hip osteoplasty. and have never had a pain free day in the last 2 years which is getting me down. i have become a hermit over this time and have now experienced weight gain as i am so debilated, i stay at home as im embarrassed by my gait i need to grip with my toes to keep me stable and walk with a limp. im a 45 year old nurse and havent been able to pass pre employment medicals, i finally secured a job as i didnt disclose my hip issues i talked myself into hiding it. i was so embarrassed i had to be honest as i only lasted 8 hours i was gutted. so i have found another ortho pod, and had another mri which showed no change from the mri i had before the last hip arthroscopy. the new report showed residual labral tearing, a paralabral cyst and now have a common hamstring partial tearing and tendinopathy. i really would love any opinion or guidance
Dear Lisa,
I believe that despite all the great effort and well-intended energy on your part and your surgical team to save you hip, clearly it has not been successful. From what you describe, you will be an excellent candidate for a THR. It’s important to find a surgeon that you trust and who will treat you and not just your X-rays or MRI.
I wish you a fully and speedy recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone,
I am a 45 year old female fitness professional since 1988 (ACE Medical Exercise Specialist, ACE Orthodontic Exercise Specialist, E-RYT 200 Yoga Pro, Star Level 3 Spinning Instructor and Kickboxing Instructor) this industry is my primary source of income and I wish to continue it for quite some time.
A little over three years ago I was diagnosed with Mixed FAI with labrum damage. I tried to manage it with strength building, stretching, etc for about 6 months but when I could no longer sit, stand or lay down I finally had to do something. I couldn’t sleep for more than two hours at a time and that was tossing and turning, popping knees and stretching quads in the middle of the night. I believe my husband was probably ready to move to another room. 🙂
I had arthroscopic surgery in Feb. of 2012, shaved and reshaped the bones of femur and acetabulum and repaired a major tear of the labrum, 8 stitches and two screws. I was so excited to complete rehab and get on with my purpose but I am sad to say that has not been the case.
From day one after completing rehab and released to resume activity I felt that something wasn’t right. All muscles surrounding hip, (QL, IT, TFL, Psoas, Quads, Hams, all Glutes, etc) were totally clamped (understandable) I was told to “Stretch the he## out of it” so I did and it continued to get worse. I was then told that I had caused tendinitis from over training and sent for injections in hip capsule and later a piraformis injection, continued to get worse. I was then told that there were three other boney protrusions in the shape of a triangle that could have been shaved but wasn’t because he didn’t think that the normal person would have the range of motion for it to affect them.
I was totally discouraged and felt that the surgery wasn’t complete. I wanted to take care of it asap but during that year I was also having major neurological symptoms and was diagnosed with a minengocyle (misspelled I’m sure) tumor at the cervical level that had penatrated my spinal cord and had to be removed right away. So the hip was put on hold during the recovery process.
Now my hip is so painful that I can’t sit, drive, lay down or sleep for any length of time. I have continued working my profession, mostly spinning, training and yoga now, but am absolutely miserable! I have a pretty high pain threshold and cover pretty well in front of clients but walk in the door or in private I very frequently burst into tears!
I was told at the initial diagnosis that I also have FAI in the other hip as well but it has just recently began to cause problems.
I’m at a loss, what is my best option now? Would a second arthroscopic surgery work for me? I don’t really want to go back to the same surgeon (he was “the best in the state”) How do I find the right one without going bankrupt? Please, any information, help, advice would be greatly appreciated!
Barbara
Dear Barbara,
I would suggest getting a fresh opinion and hip work-up. This would include plain X-rays and a good hip exam. Life is too short to be miserable. You should find out if having another hip scope would have a reasonable chance of success. More than one opinion may be in order. Ultimately you may best be served with a total hip replacement. Whether you ultimately have a total hip or another scope, kick boxing and some yoga positions may be self-destructive.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dr. Leone,
I am a 42 yr old male. I have lived a very active lifestyle, collegiate and post collegiate decathlete, and for the past 15 years an avid cyclist, everything from racing criteriums to epic 5 day 500 mile rides.
I believe my years of track and field has worn my left hip to a degree and in the past two to three years I have slowly lost some mobility and pretty much live with deep pain in my groin and a feeling of deep muscle strain/tear in my glute. I have a hard time sleeping and struggle to put my left shoe/sock on.
I had an MR arthrogram done and the diagnosis was:
scout radiographs show moderate osteoarthritis
Arthrogram showed mild/moderate osteoarthritis
Severe femoral and acetabular chondromalacia with area of full thickness cartilage loss.
Prominent femoral head osteophytes.
Synovitis along inferior recess.
Complex tear of the acetabular labrum, with tear extending from the anterior through superior labrum.
Chronic, complete tear of ligamentum teres.
So, as you can see, I feel like my back is against a wall. My stress relief and lifestyle, professionally and personally is activity driven. I have been trying to make due with a regiment of tylenol, glucoscomine/chondroitin, and an aleve, which helped for a couple months, however, I am at the point I scheduled an injection for tomorrow.
My doctor said I can be as agressive or conservative as I want, but I really want to do whatever will allow me to keep cycling and have a decent quality of life with my wife and two year old.
-I am assuming arthoscopy would not help me, however would it provide relief for a decade or two until I need a thr?
-Is there any benefit to PRP or stem cell therapy in my scenario?
-With steroid injections, are there types of corticosteroids more successful than others in my scenario?
-Do you ever privately recommend high volume/good outcome hip specialists?
Thanks in advance.
Any thoughts, suggestions, etc would be greatly appreciated.
Dear JD,
I believe that you would benefit wonderfully from a total hip replacement. I genuinely do not feel that any other treatment, such as injections or arthroscopy, will have any real benefit. Fortunately, your passion is cycling which, while vigorous, doesn’t pound or subject the joint to impact forces.. Also, be aware that having your hip injected is not without risk. I think finding a hip specialist with a great reputation, who you can trust is very important.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Im 35 and had my right hip done with an athroscophy 4 months ago. (Labrum tear, inpingement and loose bodies) Now my left groin is also starting to pain for last 2 weeks- same pain I had in right hi before. Would you recommend I get another athroscopy? DO many people need to get both legs done? Or do I wait a number of months and see if it gets any better? Many thanks
Dear Pieter,
Many times the underlying pathology that leads to the development of symptoms in one hip also is present on the contralateral side. If you are doing well with your right hip following arthroscopy, I would recommend that you have your surgeon fully evaluate you left. If you have developed similar pathology in your left hip and arthroscopy is being considered, it’s better to have it performed sooner rather than later.
I wish you well.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dr.Leone,
I have been diagnosed with a torn labral, bursitis along the outer edge of hip/thigh and impingement. Ortho states this is most likely due to the slipped epiphysis I had when I was ten. At the time a different ortho put 3 pins in and removed them three years later. I am currently 36 and have two small children, so when the arthroscopy to clean and or repair the labral and shave part of the bone was suggested I hesitate because of the recovery. I have tried PT and have been seeing a chiro to head off the inevitable but the pain has recently gotten worse after a four mile hike. My question is how long can I wait to do the surgery? The current ortho is very experienced and has already said this is to get through 10-15 years when I will more than likely need a full replacement. Does this sound typical? How can I change my day to day to helpmwith the pain?
Dear Melissa,
If you have made a decision to have hip arthroscopy then it is better to proceed sooner rather than later. As more time passes, the labral tear becomes more difficult and less predictable to repair and cartilage delamination at the labral cartilage junction becomes more likely. Once the cartilage delaminates and breaks down, long-term success with an arthroscopy is small.
Listen to your body and avoid activities or positions that cause pain. Pain is how our bodies “talk” to us, letting us know what we’re doing is not beneficial.
I wish you a full and speedy recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I am a 53-year-old male. In June 2014, I began experiencing a dull pain at the outside of my left hip, which worsened with prolonged sitting. At the time, I was active (running, cross-fit, moderate weight-lifting). Gradually, I reduced activity with the hope of getting my hip to heal. At this point, I have not exercised in six months. PT did not help. I’ve now had an x-ray and MRI.
MRI Findings:
Labrum: There is anterior superior labral tear.
Bone marrow: There is an osseous bump at the left femoral head and neck junction.
. . .
MRI impression:
1. Cam-type morphology of bilateral femurs with osseous prominence at the femoral head and neck junctions bilaterally.
2. Left anterior superior labral tear at base of the labrum.
. . .
My x-ray shows good spacing in hip joint. No mention of arthritis–one way or the other.
I recently had a steroid shot, which helped only a little.
Candidate for arthroscopic surgery?
Thanks very much,
Dear Michael,
The history you give is one is hear very frequently. Your labral tear most likely is secondary to acetabular femoral impingement. The biomechanical abnormality which lead to your impingement is genetic or has been present since you were very young.
Usually associated with this mechanism for labral tearing is delamination of cartilage at the chondrolabral junction. This is the beginning of degenerative arthritis.
I think an arthroscopy might be a consideration if there truly is no loss of joint space, an excellent quality MRI does not demonstrate delamination or chondral loss and the osseous prominence on the head neck junction would be removed.
Recognize that most 53-year-old men with a CAM type impingement with labral pathology and symptoms present for two years, don’t do well with a hip scope.
For most, THR is a more appropriate and predictable treatment option.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dr. Leone –
I am a 31 year old female. I had a ski accident in 2008 which led to a fractured vertebrae. I also fell on my hip. Since that trauma, I have had limited hip mobility (not being able to lift beyond 90 degrees without pinching). In 2013, I started to feel pain in my hip area. It did well with PT and went undiagnosed.
In 2015, I was diagnosed with FAI and PT is starting not to help much. The pinching is becoming more and more painful and my hip is achey more frequently. However, I was recently pregnant and I had ZERO pain – I think because of the hormone relaxin. In early 2015, my MRI said this:
“Trace physiologic hip joint fluid is present. Mild intermediate signal intensity degeneration of the anterior and lateral labrum without evidence of focal fluid filled tear or area of detachment. There is mild partial thickness cartilage loss of the lateral acetabular periphery at the labral chondral junction. The femoral head cartilage is preserved. The ligamentum teres demonstrates degeneration and scarring. There is normal sphercity of the femoral head with an alpha angle measuring less than 55 degrees. There is no evidence of subcortical cystic change, bone marrow edema, or cortical remodeling along the anterior aspect of the femoral head – neck junction”
There are 2 experienced arthroscopic hip surgeons in my area (the San Francisco Bay Area) and I hope to get appointments with them. I don’t know if I have arthritis, and if I do, what grade it is. However, in your opinion, am I a candidate for this surgery?
Best,
Alexandra
Dear Alexandra,
I would encourage you to be further evaluated by the orthopedist in your area. An intra-articular injection with a local anesthetic may give insight as to how much of your pain actually is coming from your hip versus another source. If it is determined that your pain and limitations are from hip arthritis, not an internal derangement such as a torn labrum, I would not expect an arthroscopy to help you. Ultimately, a total hip replacement might be appropriate, but first get a clear diagnosis and then exhaust all conservative treatment options.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello,
I’m 35 and underwent two arthroscopic labral repair and osteoplasty surgeries for a pincer impingements in both hips in 2015 (August for left hip, Oct for right). At the time of surgery for my left hip, I already had developed mild osteoarthritis in that joint. No arthritis in my right hip. I also have acetabular retroversion. I’ve been in PT since then and just started cycling, but now I suspect I’ve torn both labrums again. My symptoms are mild right now, but nearly exactly mimic my symptoms from last year at a lower pain level. I’m scheduled forr cortisone shots in two weeks but I fear they won’t help. If I did in fact tear one or both labrums, is there any chance (in your opinion) of an arthroscopic revision, or is open revision more likely? Or are either of those unrealistic and PAO or THR more likely? Thanks.
Dear Sarah,
Honestly, I suspect bilateral THR is in your not too distant future. I’m less optimistic that another hip arthroscopy will provide a real long-term solution, particularly with your left, hip due to the arthritis that was documented. That said, I think it’s reasonable to have both of your hips re-evaluated which will include repeat MRIs. Possibly a problem will be found that can be treated effectively with further arthroscopy. If you are recurrently injuring your labrum from impingement secondary to acetabular retroversion, then only PAO will fully correct it. These are major surgeries with difficult rehabs and unfortunately not as predictable as THR.
My recommendation would be to return to your surgeon and seek his or her advice. If you do decide to explore PAO, then find an orthopedic surgeon with special knowledge and expertise in this area.
Ultimately, THRs may be your final answer, but exploring all the alternatives is reasonable and will give you “peace of mind” with whatever direction you decide to go.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello,
I’d like your opinion on what you think would be best. After reading your article, I looked up the special surgical table and I gotta admit it really scared me haha.
I’m a 26 year old female who played sports her whole life. Since I was a little kid, my hip would lock on me and just hurt so bad that it would leave me in tears and unable to move. The incidents were very far and few between. My pediatrician finally decided to start listening to me when I was 16 because sports were becoming increasingly difficult, and sent me to an ortho surgeon. He took a look at the x-rays, moved my legs around, and said it was just chronic hip pain. Annoyed, I waited another 6 years before going to another ortho surgeon. He said the same thing. There’s nothing wrong, it’s just hip pain. By the end of that appointment I was very discouraged. He did send me to PT because he noticed a slight loss of range of motion and wanted me to strengthen my legs back up. Well PT was horrible. Walking had become excruciating to the point of it interrupting my work. I decided to quit because it was making things worse.
Jump forward another 4 years and I make another appointment because everything is so much worse. Constant popping, and locking on me more often. Even though it still would come and go, when it would come the pain bouts would last much longer. The last straw was when my hip locked and I was terrified I was going to pee my pants before I made it to the bathroom upstairs. I could barely move my legs half an inch. The pain was so intense and whenever I tried to put weight on my one leg I thought I was going to give out on me. Then I was going to call off work, but my office forced me to come in no matter what I tried telling them. It was excruciating to lift my leg enough to just use the pedals.
After that I made an appointment with another orthopedic surgeon. She told me there was a few things it could be. One where the head of the femur was losing blood supply, (nope wasn’t that) or something else that I can’t remember that would’ve probably required a total hip replacement. She also suggested that hip bursitis was a possibility on top of everything. Especially since laying on my side hurt a lot, and I’m a side sleeper. Well after an x-ray, she sent me for an MRI which I was thankful for. Sadly she too said there was nothing wrong, except bursitis but that wouldn’t cause all the locking and popping! But she sent me to another orthopedic surgeon that would do exploratory surgery if needed if he couldn’t pinpoint the issue.
He did a whole evaluation, which hurt like heck, and decided on giving me cortisone shots before I left the office. They helped for a week, but that was a great week. He took his own set of x-rays, and told me that he noticed that I had FAI, and set me up with some pain pills called meloxicam. Told me that he was going to send me to PT, but if it became too painful like last time to let him know and he would do surgery. The therapist told me I lost 30% range of motion in my hips, and have basically no strength. Since starting, I’ve barely made an improvement and the pain is still there, The pain from PT lasts up to 2-3 days after until it goes back to the normal pain. (Which is better than last time I had done PT because that was continuous) What would you suggest I do? I’m afraid of having surgery, not only because of what they’ll find, but because of what they may not find. I don’t want to be told again that there’s nothing wrong. Any advice would be appreciated on what it could be, or what I should do?
Dear Ruelin,
The symptoms you describe sound mechanical. Something is happening that suddenly results in your hip locking, resulting in excruciating pain. The underlying etiology must be diagnosed before it can be definitively treated.
It’s interesting that the cortisone injection temporarily helped. It is important to understand if the injection was placed inside the hip capsule (intra-articular) or externally (such as into the great trochanteric bursa). If the injection was placed inside of the hip joint capsule and you experienced significant relief, it would suggest a problem inside of your hip joint. An unstable labrial tear has to be strongly considered. Femoral acetabular impingement (FAI) can result in your labrum tearing and can account for your symptoms.
I would be very hesitant to proceed with an “exploratory” surgery. On the other hand, undergoing a surgical procedure to specifically treat diagnosed labral pathology and FAI may be very reasonable. Because your problem has be going on for so many years, understanding if secondary arthritis has developed and to what degree also is very important.
My advise to you would be to recognize that even though your problem is not obvious, it is diagnosable and then hopefully treatable. And, no, you’re not crazy. You should find an orthopedic specialist who focuses on solving hip problems just like yours. This individual may have special expertise in hip arthroscopy, joint replacement or even joint preservation.
I wish you a full recovery
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I am a 64 year old female & for 8 months have had sharp pain in my groin. At times, the pain is so severe that it almost brings me to my knees & I gasp involuntarily. That pain is also present when I get in & out of the car, and when I climb stairs. I also have pain that travels down my thigh & into the area on the inner side of my knee, along with some pain in my butt. The pain is also present when I’m in bed, and often keeps me from sleeping. My Ortho Dr. said that I have good range of motion in my joint, and that I still have a good amount of cartilage around the top of the joint. My x-ray shows moderate arthritis & some bone spurs. I have had 2 failed hip injections (guided by x-ray) and have had several weeks of physical therapy, with not much (if any) relief of pain. The hip injections did relieve my pain for the first couple of hours because of the anesthetic, but no relief after that. The Dr. said this was probably a labral tear, and I am scheduled for an MRI with contrast next week to confirm this. If this is a labral tear, it is not due to an athletic injury, as I do not participate in any sports. He also said that while he doesn’t perform a hip “scope”, another Dr. in his practice does, but won’t touch anyone whose joint is less than “pristine”. Obviously I fall into the not pristine category. The Dr. also told me that this “scope” procedure had only about a 33% success rate, so I’m thinking “why would I do this?” He did not offer me any other remedy, but said he would probably have to refer me to someone else. I would like to know what can be done for me, in your opinion, because I cannot live with the pain I am having. Thank you so much!
Dear Joan,
From your description, you sound like a very good candidate for total hip replacement. You do not sound like a good candidate for hip arthroscopy. I suspect the only thing the MRI will show is how much more advanced the arthritis is than is apparent on plain X-rays. Some patients with minimal cartilage loss still have disabling symptoms and only are helped after THR. X-rays do not always tell the whole story. It’s important to not treat the X-rays but rather the patient.
My advice is to return to your doctor and further discuss your symptoms and complaints. I would suggest you specifically discuss THR. I encourage my patients to seek other opinions if they have any reservations regarding my recommendations.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Thank you so much, Dr. Leone! I do have an appointment coming up with the Dr. and will bring up THR with him. I’m hoping my MRI results will aid him in deciding what the best way to proceed would be for me. After reading everything I could get my hands on about my situation, it doesn’t seem like I would be helped by the athroscopy procedure.
Thanks again for your time!
Hi, hoping you can give me some advice/direction.
My symptoms are minimal pain on a daily basis – worse with activity or sitting for awhile, stiffness and lessening but bot severe rom. Some nights, maybe 1-2 per week i need to take anti inflamatories and pain killers which helps.
My mri states mild pincer type morphology, mild chondrolabral delamination signal abnormality anterosuperior quadrant acetabular articular cartilage surface, small undisplaced anterior labral tear, mild gluteal tendinopathy and trochanteric bursitis.
Any advice on next step i should take?
Dr Leone,
I am a 59 year old former tennis player with FAI on MRI and a possible labral tear (not seen on MRI, but suspected due to groin pain, length of pain and location). I have classic deep groin pain and exacerbation upon walking hills, stairs. To complicate things, i have significant lumbar stenosis on MRI leading to leg weakness, so the hip pain was being attributed to the leg weakness and spinal issues. A fusion has been recommended by the neurosurgeons, but they agree it would not address my hip pain, which is my major complaint. I have decided to only address the hip issue surgically as I have little to no back pain. My leg weakness is better with PT. As of my plain film a year ago, I did not have significant arthritis of the hip, the only findings have been on MRI (FAI). I do not have anywhere as much pain upon sitting or laying down. I am scheduled for arthroscopy in a few months. I know I will be on crutches for while. I understand that outcomes of THR are often better than arthroscopy so I am questioning my decision. I am going to have another MRi since its been 17 months. My mom has had bilateral hip replacements. Do you think it makes sense to consider a THR when I dont really need it now, but the arthroscopy doesnt have as good results and the recovery is actuallly easier for the THR? I also wonder if the arthroscopy could hasten the need for a THR and dont want to be taking so much time of work to have multiple surgeries. I appreciated your input. thank you
I am 46 and live for tennis. I was recently diagnosed with a labral tear: “anterior superior labral nondisplaced tear.” I guess I’m lucky because after resting and getting PT for 4 weeks, I have no issues walking, sitting, etc. I don’t know whether I can get back to tennis; the PT says he thinks the side motions might cause the pain to return.
I assume the tear is small (my former ortho didn’t spend any time going over the results so I have an appointment with a different ortho). I have good range of motion and none of the doctors, PT’s or chiropractors I saw thought it was a tear because the movement tests didn’t elicit pain. My MRA report says that a small amount of the contrast material extended into the anterior labrum superiorly but the rest of the labrum appears intact. Hip alignment normal; bones appear normal; cartilage surfaces appear intact; no acetabular protrusion, retroversion, or abnormal morphology of the femoral head. Muscles, tendons and ligaments look fine. The ortho said upon examining X-rays that I have good spacing within the joint.
I am assuming that the new ortho will want to keep up PT. I’m ok with that, and am willing to reduce the amount of tennis I play and/or work with a tennis coach or therapist who can help me change my stance and footwork to reduce hip strain. I am overweight so I’m working on weight loss now. I just can’t envision a world with no tennis.
Does it sound like I might be a candidate for arthroscopy? I would prefer to go the PT/retraining route if possible. Are you aware of success stories of returning to sport with just PT? Finally, I have read that many tears are asymptomatic. Is it ever possible that a new tear can become asymptomatic? Or that the tear was already there without me knowing it, and that I had another injury that caused the tear to become symptomatic?
Just not sure what to do…
Hello, I am a 65 yo male living in Colorado. I have been a very active cyclist for many years but about 2 years ago I started experiencing pain in my groin when riding. I was able to complete 2 multi day rides in the mountains in the summer of 2014 with the aid of a cortisone injection. In 2015 I tried to complete the same level of riding and found that the pain in my hip was much more extensive (despite more cortisone) and limited my abilities. I had an MRI and xrays and was diagnosed with cam impingement and a laberal tear. I’ve spent the past 6 months working with a PT to see if I could resolve the hip issues but things are no better and I’ve done very limited riding this summer. Just to be clear, my main issue is being able to return to my former level of cycling activity but I now have pain on and off the bike.
I have all along assumed that I may run out of alternatives and require arthroscopic surgery. However, I met with a hip arthroscopy surgeon yesterday and he suggested, somewhat reluctantly, that, given my age, an anterior THR might be a better alternative. I find this to be a very attractive idea since I can expect to require at least 6 months to fully recover from the arthroscopic surgery with a procedure that has a lower chance of success and may induce arthritis that could require a THR in future. At this point I am not a typical candidate for THR. I have only slight arthritis and the bone spacing is good. But the much higher probability of success and a much shorter recovery time are very important considerations for me. What is your advice?
Dear John,
Most 65-year-old men have a more predictable and satisfactory outcome following total hip replacement rather than hip arthroscopy. Usually, there is more arthritis present than one can appreciate from pre-op studies. This is especially true considering your hip problem has been going on for several years. The approach used to implant the THR is much less important than the individual surgeon you chose to do the surgery. What is most important is that your hip is expertly implanted, that hip mechanics are optimally restored and tissues are meticulously handled.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello, My name is Stephanie and I am a 54 year old runner. I had a partial hamstring tear 2 years ago and could hardly sit while driving; I did have an mri and I do have cam and pincer impingement in my hip with bone spurs. A year and a 1/2 ago I had ultra sound guided steroid injection which did help for about a year. Just saw my doctor on Friday and he did say that my hip has gotten worse. I decreased my running from 50 miles a week to 25 miles a week. He gave me another injection as I am now experiencing pain when I walk up steps. My question is would an arthoscopic hip surgery help clean out all of this and shave extra bones so I can decrease the degeneration in my hip and I can continue to run? Thank you for any advice
Dear Stephanie,
Unfortunately I do not believe a hip arthroscopy would provide any real long-lasting relief. In fact, it probably will not provide any short-term relief either. The fact that your orthopedic surgeon told you that your hip looks worse, suggests that the hip joint space is less than it was just 18 months ago. You have an arthritic hip with mechanical abnormalities (cam and pincer impingement) that lead to the arthritis. At some point, this condition can be treated very effectively and predictably with total hip replacement.
I think a reasonable strategy would be to look for those activities that don’t accelerate the destructive process while allowing you to remain active and as pain free as possible. The repetitive impact of running is not beneficial to your degenerative hip. I would consider other exercise such as biking or swimming. If something hurts, you’re not helping yourself.
The occasional intra-articular cortisone injection is effective but will become less effective with time and with each successive injective. Hip replacement surgery should also be delayed at least three months after your last injection to diminish the risk of a post-operative infection.
I wish you the best,
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dr. Leone,
My wife is 69 yr old. She has labral tears of both hips but the left side is worse causing daily discomfort. It limits her ability to walk anything but short distances and causes pain when sitting for extended periods of time (excess of an 45-60 mins.). She has had two steroid injections for the left labral pain which did not help. She also has very minimal arthritis. She has been rejected as a candidate for arthroscopy by two local sports doctors due to her age and arthritis. She doesn’t think she’ll be taken as a candidate for THR for another 10 years when her arthritis gets “bad enough.” What advice do you have for her?
Dear Tom,
Your wife is 69 years old and suffering now. It’s been my experience that the arthritic condition is almost always worse than expected when viewed at time of surgery. It’s also been my experience that hip arthroscopy has a poor track record in older individuals with labral tears because of the underlying arthritis. I’ve always maintained it is important to take care of the person, not just go by an X-ray. My advice would be to have your wife explore total hip replacement.
I wish you and your wife the very best.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello,
I have been diagnosed with some arthritis… cam impingement and labral tear in my right Hip about 3 years ago, it says there is a partial replacement of the superior/lateral labral by spur with cystic change which could related to a paralabral cyst which has dissected into the bone. there is spurring at the right femoral head neck junction noted. Spurring along the acetabular margins bilaterally with degenerative changes could be reated to chronic impingement. Now I have Trendelenburg Limping. I have also noticed that my right leg foot faces outward..When i walk my right foot goes outward and my weight comes down on the outside of my foot, not heal to toe. I never walked like that before this happened around three years ago. I have had pain all over my hip..right hip pain and side hip pain..felt the my groin heat up when it first happened. Hip is always very tight especially when sitting. Its been three years, I am 60 years old. I might add i have had 2 MRIs without contrast that showed this. My question is should i have another MRI with contrast this time and do you recommend a total Hip replacement? I am at my witts end. I feel like half a person. Tired of the pain and do not feel balanced. Thank You So Much.
I am 54 and a former runner of 35 years. I had an hip injury after a marathon three years ago, and after some PT (which did help- doctors at the time weren’t convinced I had a labral tear) tried to go back to running lightly and then developed hip flexor tendinitis bilaterally. I biked for a while and pain improved. Now a year and a half later, the pain in my hip is back, not only on exercise (of which I do very little now other than walk and 20 minutes on elliptical) but also at rest. I still have the tendonitis (including calcific tendonosis of sartorial muscle) and the doctor thinks I have trochanteric bursitis bilaterally. I have mild hip arthritis with evidence of a cyst and degenerative labral tear. I also have osteoporosis. What would be your recommendation? Another course of PT? Cortisone injection? (Given that I have osteoporosis in hips?) Thanks.
Hello Doctor,
Amazing that you are giving this input to people. Thank you.
I am 46, and developed hip discomfort in the past 2 months. Although I am walking normally with almost no pain, certain movements cause a very unpleasant jolt.
I am quite active: swim, pilates, run, mountain bike, ski.
I had an MRI and x-rays, and saw three different doctors.
The first said I had a labrel tear and should operate immediately, including shaving my femur due to FAI. He said that continuing to exercise (I have a big ski trip planned) could cause articular arthritis, which is not curable.
The second said I shouldn’t bother getting arthroscopy, as the MRI showed that I had already lost too much of the underlying cartilage. Opening the hip up to do arthroscopy could “push the hip over the edge.” He suggested just trying to ride out my hip for as long as possible, and then get a THP, likely in my early 50s. I could go on my ski trip, because it didn’t really matter anyway.
The third said that was nonsense. That the 2nd doctor only likes to do hip replacements, but that he thought I didn’t have too much underlying cartilage loss, and that if I did, he could do micro-fracture (the 2nd doctor said micro fracture didn’t work well). He would also shave a big bone spur I have on the hip. I could ski because my labrel and cartilage damage was done progressively over decades, and another 3 months wouldn’t make a big difference.
So I have 3 overlapping, but different views. Each, I’m sure, is genuine in offering his assessment. The question appears to be: I have some articular cartilage damage; but do I have too much to risk getting hip arthroscopy to prolong my natural hip and delay a THP?
How do I, as a patient, ascertain if my hip can absorb the trauma of arthroscopy and heal properly vs. being damaged, and hastening its collapse?
It doesn’t go with my life ethic in general to just let things degrade. I can exercise to support the hip. But doing nothing and just waiting for the pain to get worse isn’t very inspiring.
Do you have any guidance on how I can cut thru these opposing views to get at the safest path forward for me? I liked what the 3rd doctor said to me, but if he’s wrong, I pay the consequences.
Thank you.
Shayne
Dear Shayne,
My experience has been that 46-year-old, active guys with early hip arthritis and underlying FAI don’t do well with hip arthroscopy. Hip arthroscopy is not without risks and I would consider seeking further opinions. I also would try to figure out what exercises and activities you can do that don’t subject the joint to a lot of impact, which potentially could progress the arthritic condition.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Question: I have bilateral hip bursitis (both hips). First round of steroid injections provided relief for 2-1/2 months, second round of steroid injections did nothing. I have tried physical therapy and cannot take anti-inflamatories because of reoccurring stomach ulcers. Even if the steroid injections worked the second time I would not be a candidate for continuing because I am a diabetic. I also have left hip impingement as well. My Orthopedic doctor does not “fix” that and says I need arthroscopic hip surgery performed by someone who specializes in that.
Question: Do people have both hip bursa sacs “shaved” at the same time? Do you recommend?
Also, I have two prolapsed organs (bladder/rectum), would you recommend fixing that before or after fixing hips? Just wondering legs in stirrups for extended surgical time.
Thank you,
Dear Dr. Leone,
Thank you for providing this forum for better understanding FAI and possible remedies. I am 56, very active with tennis, cycling and swimming. About a year ago I noticed general hip instability for lateral (to the left) movement on the tennis court. In June I noticed a hip click when standing. The pain and ache for clicking became more pronounced in August. After X-rays and MRI the diagnosis is still inconclusive but there is an edema in the socket which perhaps indicated cartilage damage. I have “early minimal arthritis” according to the radiologist report. There was so much swelling in the joint the swelling was causing a number of secondary problems but after 3 weeks of extreme rest and Aleve the swelling has subsided and now I feel a sharp pain as I sit — like crushed glass in the joint as I pass through a 30 degree angle towards sitting. I’ve tried PT with no relief. It seems like I would be a candidate for an arthroscopic solution — can you confirm?
Hi Dr. Leone,
I am a 34 y/o female. I am very active – marathon runner for 14 years and am on my feet all day as a primary teacher. After having debilitating pain on my right lower body, I started seeing a chiropractor 2 years ago for what I thought was sciatica. I had extreme pain in the hamstring and periformis. After much adjusting, ART, etc. one year ago I ended up with an avulsion fracture from my hamstring still pulling on my hip so hard. After a 2nd MRI with dye, the findings say “pincer-type morphology with mild degeneration or anterior superior labrum. No labral tear.” My lateral center edge angle is only 42 degrees opposed to the normal 39. The surgion suggests athosocpic surgery to shave the bone on both areas of the socket and to trim the labrum. I am scheduled for the surgery in less than two weeks but I feel this may be “jumping the gun” based on the mild damage. I am afraid this surgery will not fix the pain that is debilitating me currently. My current pain in down the back of the leg, the groin, and seriously in the SI joint and hamstring. Do you believe this surgery is necessary? Any advice? I am so unsettled about this all.
Dear Carrie,
The mechanical problem which led to your symptoms needs to be corrected. It sounds like your surgeon is planning to do this arthroscopically. Hopefully, he or she will not discover significant arthritis (destruction of hyaline cartilage) which is not easily treated. You are disabled now with your hip symptoms. If the arthroscopic surgery fails, and you remain this disabled, then most likely you will consider a future THR. In someone only 34 years old, I think it’s reasonable to try all options and treatments to solve your problem and hopefully prevent or delay THR.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Carrie,
The mechanical problem which led to your symptoms needs to be corrected. It sounds like your surgeon is planning to do this arthroscopically. Hopefully, he or she will not discover significant arthritis (destruction of hyaline cartilage) which is not easily treated. You are disabled now with your hip symptoms. If the arthroscopic surgery fails, and you remain this disabled, then most likely you will consider a future THR. In someone only 34 years old, I think it’s reasonable to try all options and treatments to solve your problem and hopefully prevent or delay THR.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Thank you for this article! I am a 42 yo F who underwent an arthroscopy for a labral tear 4 months ago. In addition, I also had femoral neck shaved and cyst removed. My first consult was with a surgeon who did not repair torn labrums and referred my to another practice. They did, however, try a cortisone injection which did little for any relief. They also performed the initial xray and arthrogram for diagnosis of labral tear and dysplasia. Surgical consult with surgeon who could repair labrum did not review xray only arthrogram and did not seem to be concerned with the dysplasia.
At a follow-up at 8 weeks PO, it was determined that the arthroscopy resulted in accelerated arthritis leaving me now bone-on-bone with a frayed (formerly “repaired”) labrum. How does this happen? Is my only course of action now a THR? I can no longer walk without assistance and in constant excruciating pain.
Thank you, in advance, for any advice/suggestions/explanations.
Dear Elaine,
Yes, in all probability you will greatly benefit from total hip replacement. My recommendation would be to focus on finding an orthopedic surgeon who you trust to perform the surgery and care for you. Mentally and physically prepare pre-operatively and then fully rehabilitate afterwards to “get your life back.”
I’m sure that your physicians who tried to help you did their very best to relieve your pain and preserve your joint without total replacement. Sadly, it appears to have failed. You should feel good that you did everything within your power to recover. Now go on with a positive attitude and a great prognosis for the future. I would not look backward.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.