The Unhappy Total Knee Replacement Patient: Figuring out What Is Wrong
“Do I Have The Wrong Size Knee?”
Unfortunately, there are a significant number of people who have undergone total knee replacement (TKR) and are not happy with the result. Some studies estimate 20% or more fall into this category. Defining success or a “satisfactory result” can mean two very different things to an individual who had the total knee versus the surgeon who implanted it. At the end of the day, it’s most important that the person who had the TKR is happy.
Defining “success” for the TKR begins even prior to surgery, during a frank discussion between patient and surgeon, with regard to what that patient’s goals are and if the surgeon thinks those goals are achievable and appropriate. Some goals simply are not reasonable, such as long distance running or team soccer, particularly if the new joint is to enjoy longevity.
When a patient is not happy with the result after surgery, it is very important that we understand why. Many times, the specific complaints give clues as to the underlying problem. Ultimately, if the situation is to be rectified and the problem corrected, then the specific etiology must be clearly delineated. TKRs work wonderfully, but only when a host of important variables comes together. I call these “the surgeon’s goals” which is what I try to achieve during an operation and, when accomplished, helps assure a stable, pain-free knee with which the patient is happy.
- Recreating limb alignment and a neutral mechanical axis so that weight-bearing forces are nearly equalized between the inner and outer compartments of the knee. This also has the effect of straightening any pre-TKR bowlegged or knock-kneed angulation.
- Balancing the soft tissue sleeve that surrounds the knee so that as the knee moves from extension to flexion, equal and physiologic tensions or pressures are experienced in the medial and lateral ligaments.
- Creating normal knee movement or “kinematics” as the knee ranges from extension into flexion and then back to extension. Normally, as the knee flexes, the tibia internally rotates and the femur pivots on the inner or medial compartment. During extension, this normal rotation or pivot reverses and the tibia externally rotates. The cruciate ligaments as well as other soft tissues and the shape of the bones help to control this normal complex movement.
The components implanted during TKR do a wonderful job of re-surfacing the end of the bones that make up the knee and this prevents the bones from rubbing. “Bone on bone” pain is one of the main reasons why arthritic knees are painful and a major trigger for patients deciding it’s time to choose knee replacement. For the result to be optimal after TKR, these three conditions need to be met. This can prove very difficult to accomplish consistently, especially with some patients’ particular deformities or underlying conditions.
The search for the etiology as to why a specific patient is not happy begins with a careful history. I inquire regarding what the original diagnosis was prior to the knee replacement and try and get an idea of how disabling the condition was. Was the person barely able to get up from a seated position and walk or did they have just a little discomfort after 54 holes of golf? I also ask if there were any problems with the incision after surgery or any need to return to the OR, which might increase the suspicion of an underlying infection. Were antibiotics extended after surgery or initiated after discharge? Many infections are subtle and difficult to diagnose.
What is the main complaint? Possibly pain, stiffness, poor range of motion, or feeling like the knee is not stable and that the patient can’t trust the new knee. Some patients have subtler complaints such as the “new” knee simply is not comfortable or “doesn’t feel natural.” If they’re experiencing pain, is the pain only with activity such as walking, or is it present all the time, even at rest? Does the discomfort awaken them from sleep? Can they do something that improves or relieves the pain such as assuming a particular position with the leg, using ice or pain meds, etc.?
I need to understand if there was ever a period where the patient seemed to be doing well or at least improving and then the circumstances changed. Are their symptoms now slowly improving, stable or worsening? Are the complaints tolerable or are they bad enough that the patient wants more tests, hoping to learn the specific etiology and would even consider more surgery if the condition could potentially be improved? Of course, these are just a sampling of questions that must be explored if the underlying problem is to be diagnosed and corrected.
Examining the knee is equally as important. Is knee alignment acceptable? Did the incision heal satisfactorily? Does the skin overlying the knee appear red and hot? Is the knee tender? If so, where? Is there any drainage? Does the knee appear swollen? Is there an effusion (fluid in the joint)? Does the knee fully extend? Can the person actively maintain that extended position? How much does it flex? Is this range of motion associated with pain or is it painful only in a particular position? Is the kneecap tracking or does it slide off to the side during flexion? When stressing the knee, is there more laxity on one side compared to the other?
It is important to test for stability with the knee in extension and various degrees of flexion. The anterior (front) / posterior (backward) stability also needs to be established. Other conditions that can cause knee pain must also be considered and ruled out, such as spinal disease and hip disease with referred pain to the knee. Once again, this is just a sampling of information that the physical exam can provide, giving clues as to why the result is not acceptable and to help determine the next steps to correct the problem or problems.
Good quality X-rays, including an X-ray taken with the person standing (which physiologically loads to the joint) and occasionally also including a full length X-ray that includes the hip and ankle are important. These X-ray images give important information regarding component alignment, sizing and if the joint appears stable or loose. X-rays also reveal what type of method was used to fix the components to the bone. Were the components cemented or press-fit with the hope that stability would be achieved with bone ingrowth? Do the interfaces where the bone contacts either the cement or prosthesis appear acceptable or is there a suggestion of loosening or osteolysis (bone destruction)? Accessing the equality of the inside and outside prosthetic joint space might give clues regarding soft tissue balance. Does the patella appear to be tracking centrally or is it pulled to one side? Are there residual bone spurs, which could be causing irritation or inhibit motion? As with a thorough history and physical exam, very important information can be gleaned from good quality X-rays. Similarly, a review of the X-rays that were taken prior to TKR also gives clues regarding the knee’s pre-operative deformity, appearance and underlying anatomy. Reviewing X-rays that were taken very soon after the index surgery and comparing to the most recent X-rays allows me to compare and look for subtle changes.
At this point, many times the surgeon will have a pretty good idea of what is causing the problem. Further X-rays might be necessary as well as other studies such as blood work, including an ESR and CRP.
The surgeon might suggest aspirating the knee to look for evidence of infection. Joint infection is often a difficult diagnosis to make. A new test has recently become available called the Synovasure™ test. Synovial fluid is aspirated and sent to a special laboratory where specific tests are performed. These include measuring a biomarker called alpha defensins. Biomarkers are proteins that act as the body’s natural antibiotics and are present when the body is fighting infection but not present in other conditions that can mimic infection. The Synovasure test has greatly improved our ability to diagnose infection and helps differentiate inflammation and other causes of knee pain from infection. Occasionally, the surgeon will request a bone scan, radioactive WBC labeled scan, or MARS MRI. In my experience, these studies have not been that useful. In special circumstances a CT is ordered to help better understand component positioning.
A review of the surgeon’s operative report is important. This report could give clues regarding specific difficulties or peculiarities that were encountered during the operation. The surgeon also needs to review the “implant record.” Like the operative report, the “implant record” is also a permanent part of the medical record and contains labels provided by the manufacturer naming the company that manufactured the implant, the implant brand name, size, FDA number, and expiration date. This information becomes critical if more surgery is being considered and also might give a clue as to why the knee is not performing satisfactorily. Particular bands or types may have known problems and a poorer track record than others.
If a specific etiology for the dissatisfaction can be defined, then a specific plan can be developed to address it. Depending on the diagnosis, this plan may be surgical or nonsurgical.
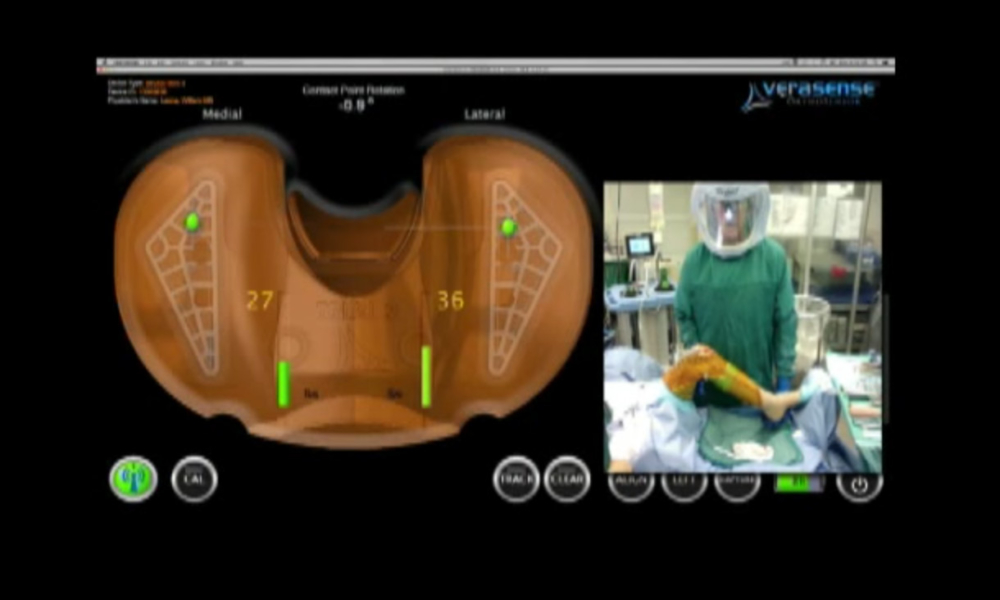
In my next article, I will discuss revising a TKR and a powerful new intra-operative tool which I use that can help me diagnose and treat subtle component positioning and balancing problems and then direct very specific soft tissue releases, bone resection and component changes to correct these problems.
As an update to this article I have written a blog article for those who are specifically concerned about symptoms of a wrong size knee.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.










My TKR is about 15-20 degrees out of alignment. Any surgeons in Atlanta who will fix this as an Atlanta Orthopedic did the original surgery?
Dear John,
If you think there is a mechanical problem with your TKR that is preventing you from fully rehabilitating, then I would suggest you discuss these concerns with your surgeon and ask him or her what would be recommended. If more surgery is recommended, then either your surgeon will feel comfortable doing it or not. If the decision is to treat you further, then you must decide if you still feel confident enough with your surgeon to remain under his or her care or would feel more confident with someone else. Regardless, I think it is always a good idea to seek several opinions, especially when the result is less than optimal. If you’re not comfortable having your original surgeon continue to treat your knee, then you need to find another, either locally or out of the area. We are so fortunate that we live in a country with many excellent physicians.
I wish you a full recovery.
Sincerely,
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I had my TKR done on October 1 2015 and a manipulation done 5 weeks later due to declining results in flex and extension numbers. The doctor only got 115 bend under anesthesia and I have continued to go to PT at least 3 times a week and my numbers at rest are 90 bend and -17 on the straightening. I am very frustrated as I had my left knee done 3 years ago by the same doctor and it has been fantastic. it just feels like I have a block of wood in there and experience severe pain when PT pushes it to 107. What can I do,I am very discouraged and frustrated and my surgeon now says he really does not know what his next step will be.
Dear Paul,
I would continue being diligent with you PT and follow up with your physician. If you continue to fail with improvement in your range of motion, then you may require more surgery to address this. I would discuss your concerns and the plan going forward with your surgeon.
I wish you a full and satisfactory recovery.
Sincerely,
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Almost one year since TKR on left leg. Worst pain I have ever experienced in my life,first three months, down to a low moan by six months, very little pain as long as I dont walk last six months. First six months felt like a basketball on top of my knee, next four months like a tight band above knee, now totally stiff. Swollen to ankle walking or laying for months, now only walking. Can not walk without tightly binding above knee. Went to physical therapy twice nothing wrong with the knee itself except only have 90 degree bend. Have noticed left leg appears to be longer than right. Right knee totally gone but will not have surgery. Can not walk through Walmart need a cart. My surgery said he had one case like this before and sent me back to physical therapy, therapist said nothing wrong with the knee. GP said to see another surgeon, feels there is a problem. Is there doctors that specialize in complications from TKR? I live in Houston. Thanks
Dear Peggy,
Unfortunately 20 to 30 percent of those who undergo TKR are not satisfied with their results. For many who fall into this category, it is secondary to subtle soft-tissue imbalance, component malposition or limb mal-alignment. If you are not doing well, almost certainly there is a specific etiology. If the exact reason for you poor result can be defined, then it can be addressed. I would suggest a further evaluation. If your treating surgeon has not been able to identify the problem, I also would recommend you find a specialist who can.
Infection must be ruled out. If other causes such as loosening or gross mal-alignment are not apparent, in my practice I’ve had great success diagnosing subtler problems by using the VERASENSE OrthoSensor, which provides quantifiable data for analysis and then directs correction. If you’re this uncomfortable and dissatisfied one year after your surgery, I would encourage you to continue to pursue further diagnosis and treatment. Most likely, it will be surgical.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I have a question. I had a partial knew replace Dec 2014. And ended up having a total knee in March 2015. Well it’s been a year and 4 months. And my knee still gives me pain. I cannot sleep. It aches badly. And there is pain that shoots down it. Not olny that but it is swollen. And it makes a awful noise. Like its loose. And no one elce knee does this. My SURGEN is retiring. Can u help with any info?
Dear Angel,
I’m sorry to learn that you are struggling with you TKR. Converting a partial knee to a total knee does add surgical complexity and I suspect that you are continuing to experience discomfort from less than optimal soft-tissue balancing. Many reasons can cause your symptoms. A further work-up to define the exact etiology of your dissatisfaction and pain is appropriate, which includes trying to rule out an underlying infection.
My recommendation would be to return to your surgeon to share your frustration and difficulties and ask for advice. If your surgeon is unable or unavailable to help you, then I would seek out other orthopedic surgeons in your area with a special interest and specialization in complex total knee issues.
I wish you a full and satisfactory recovery,
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I had a bilateral tkr 18 months ago after AVN from high dose steroids & have been back to work for 10 months. My R is perfect, no complaints but my L has increasingly become more painful. It feels like a tendon or ligament ended up in the wrong place, upon flexion/extension in get a popping feeling that causes pain, & a ice pick pain in the knee itself along with increasing stiffness the longer I’m on the knee which is all day & sometimes pain while sedentary. My goal was to just be about to work, I’m a Medical Assistant & on my feet alot. Could this just be normal pains or a greater issue?
Dear Bonnie,
From your description, I suspect that you might have a mechanical problem with your left knee. Considering that your right knee feels “perfect,” I would expect your left knee to feel similar if the construct and soft-tissue balancing were the same as on the right side. Your description of the symptoms worsening rather than improving with time and “feeling like something is in the wrong place” further supports my concern.
Technically, it is difficult to consistently and optimally implant and balance a TKR. Small degrees of component malrotation and/or soft-tissue imbalance can lead to compromised results and pain. It is reported that 20% or more of individuals who have a TKR are not satisfied. If this is what is going on, then diagnosing and correcting the problem can lead to a good result. Diagnosing the exact etiology is not always straight forward but is important.
I suggest you return to your surgeon and share your continued concerns and complaints and look for his or her advice regarding how to solve it.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello Dr. Leone,
I (male, age 58) had a left-knee TKR in December 2014, after 4 separate arthroscopic procedures over the prior 30 years had finally left me with consistent bone-on-bone pain. You write-up is wonderful, and your “surgeon’s goals” are tremendously insightful – I thank you, and wish MY surgeon had had the sense of duty and trust to discuss these with me at some point, either before OR after the surgery. Let me just add one more for your consideration, from the ranks of the unhappy: “- Avoiding adding insult to injury by cheerfully advertising how happy you’ll be if you allow our group to do your TKR…showing supposedly satisfied patients skiing, hiking, playing sports, etc…with big smiles on their faces”
Since my surgery, I’ve had a muffled “triple clunk” that causes discomfort whenever I bring my leg forward as I try to walk normally (which was the entire goal of the TKR – my expectations were very low). It is impossible to simply “walk through it”, as the body instinctively recoils, and I end up limping. When I ride a bicycle, there is a sharp muscular (I think) pain on the outside of the knee with every “push” stroke..which I do indeed try to just plow through, as I do have seemingly fine strength and range of motion. My skin is very sensitive; I cannot kneel on that knee at all.
In short, I seem to be no better off now than I was before the operation…which is really, really frustrating – especially when all I ever get from the surgeon is “Everything looks good – there’s nothing left to do.” I have a feeling I’m a victim of “soft tissue” complications, with something just rubbing the wrong way against the components.
What does this sound like to you? What would you look at as far as trying to alleviate this pain/condition? Besides an MRI (I’ve had two), are there other diagnostic tools or methods that could help shed light on what’s going on? I’ve got many years ahead of me…to think that this is “as good as it’s going to get” is depressing indeed.
Thank you for any advice/information.
I underwent bilateral TKA in March 2012. The first year was the best, then I developed effusions and patellar clunk syndrome which made the knees feel tight & uncomfortable with flexion. In February 2015, I underwent bilateral arthroscopies with resection of scar tissue. I experienced significant improvement in ROM, but then the stiffness & effusions have returned gradually along with patellar clunk syndrome on the left. I achieved 120 degrees of flexion after the original surgery and after the arthroscopy, but now it is about 90 degrees. I cannot ride a bicycle or get out of a chair without using my upper body. Hiking, a favorite activity is very uncomfortable when walking downhill. I am very unhappy with the limitations of my knees, especially since I worked very hard on my rehab following the original surgery. Do I need revisions?
Dear Alan,
Patella clunk syndrome refers to a condition that can occur after TKR when excessive scar tissue develops at the quad tendon insertion into the patella. The scar tissue nodule catches on the anterior edge of the femoral component, typically when the patient extends the knee against resistance, such as getting up from a seated position. The fibrotic nodule releases suddenly with a painful clunk, as the knee extends. Many patients will develop some degree of anterior knee crepitus or a palpable grind after knee replacement, and if not symptomatic, it does not require treatment.
The condition more typically develops in those patients who achieve high degrees of flexion after a knee replacement (>120 degrees), is more common with certain knee designs like posterior stabilize (PS) > cruciate retaining (CR), when a patient has patella baja (when the patella is low riding or more distal relative to the joint line than normal), or when the femoral component is excessively prominent or flexed, and occasionally when the total knee reconstruction required correction of significant angular deformity.
When patella clunk syndrome develops and is symptomatic, quad strengthening and consideration of an intra-articular cortisone injection into the knee is reasonable. If this fails and symptoms persist, the condition is often treated successfully with debridement of the nodularity either arthroscopically or with open surgery. If following debridement the condition returns, I think a critical re-assessment of any underlying condition that may be leading to persistent irritation of the quad tendon and to the development of the condition needs to be understood and then addressed. If there is a mechanical problem or soft tissue instability underlying your recurrent problem, then that needs to be corrected in order to ultimately resolve your condition.
My advice is to return to you surgeon and share your frustrations and symptoms. Look for his or her advice in how to resolve it. I think it’s always reasonable to get other opinions from different knee surgeons who may have a different perspective or experience.
I wish you a full recovery
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I am in MI and have had both knees replaced, two years apart. The first one is perfect. The second is horrible. I have been told it is a problem of growing too much scar tissue. I went back in 6 months post surgery and had the scar tissue surgically removed and started all over again with the CPM machine and PT. After 3 months of PT 3 days a week I was stopped by the scar tissue again. I ended up waiting 6 more months, hoping it would work out. It never got better. I had sedation and manipulation and left right from the surgical recovery to PT. I used the CPM machine (again) and 3 days a week for 3 months in PT. The Physical therapist just threw up his hands and said that I was not going to get better than this. I bearly can bend to 90 degrees. I have a hard time sitting down and getting back up. I have trouble getting dressed, can’t make it all the way through grocery shopping. My quality of life SUCKS!! I don’t know what to do or who to see next, but I cannot go on like this. Please help.
Dear Lisa,
The fact that your first TKR has done so well and your second did not begs the question, what is the difference between the two? Understanding the difference is the key to ultimately solving your problem. Was the same manufacturer and prosthetic knee used for both reconstructions or were they different? If they were different, how – the size of the components, type [cruciate retaining (CR) versus posterior cruciate substituting (PS)] and composition of metal used, cobalt chrome versus titanium/oxinium? Alignment? Soft-tissue balance and restoration of the joint line? All of these should be assessed and compared to the well-functioning TKR. Infection, though unlikely, also needs to be ruled out.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I am in MI and have had both knees replaced, two years apart. The first one is perfect. The second is horrible. I have been told it is a problem of growing too much scar tissue. I went back in 6 months post surgery and had the scar tissue surgically removed and started all over again with the CPM machine and PT. After 3 months of PT 3 days a week I was stopped by the scar tissue again. I ended up waiting 6 more months, hoping it would work out. It never got better. I had sedation and manipulation and left right from the surgical recovery to PT. I used the CPM machine (again) and 3 days a week for 3 months in PT. The Physical therapist just threw up his hands and said that I was not going to get better than this. I bearly can bend to 90 degrees. I have a hard time sitting down and getting back up. I have trouble getting dressed, can’t make it all the way through grocery shopping. My quality of life SUCKS!! I don’t know what to do or who to see next, but I cannot go on like this. Please help.
I had A TKR 2010 when I was 21 because of Arthritis. My knee is getting deformed (bow legged) and it causes a lot of pain. I feel it’s going to snap to the side.I try to use a brace and it helps a little. Is it because of my weight or am I due for a replacement? And if I do get a new TKR will it help with the pain and defoemity.What do you think I should do?
Dear Isabel,
It is unusual for someone as young as you to already have undergone a TKR. The underlying reason that required you to have TKR in the first place needs to be understood, i.e., rheumatoid, tumor resection, trauma, etc.
It is very concerning that your knee is developing progressive genu varus (bowleg) deformity and that it is causing pain. Total knees, which are well balanced and aligned, last for many, many years even in someone your age.
What you describe now will only get worse. Therefore, I suggest you return to you surgeon and share your concerns. I do suspect you will need further revision surgery. If you are significantly overweight, then it behooves you to lose weight, which hopefully will improve your chance of a good outcome.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible
I had my Tkr done March 14 2016. To this day I still have swelling, stiffness n pain. I do my exercises everyday, stretching n pulling on that knee to the point of tears. I mix up my strength exercise n walking n stationary bike n pool every other day. I’m doin all I can. My flex ion about 3-4 weeks ago just after pt was 110/2. My question is, if I keep up with my exercise program, will my rom get better. This surgery can be very debilitating physically n mentally. I’m very frustrated. I didn’t sign up for these results. My surgeon said wants to see me in another three months. He never says too much, about ” where do we go from here”? Do I have hope for better results? Are there other options to remedy my low bend results? Thank u for any information
Dear Kathy,
Fortunately, the range of motion (ROM) and functionality of TKR can improve over the first one to two years.. My advice would be to “hang in there.” If after a year, you still are frustrated and not happy, then consider what else can be done to improve your result. If in the interim your results are worsening (that is, you are losing ground with less ROM and more pain) then look for solutions or other opinions sooner.
I wish you a full and satisfactory recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I have had both tkr 3 mo apart. Right knee may 2016 was great at 6 weeks post op I was 130-135 and 1% straightening the leg. I am 7 weeks post op on my left knee it has great flex also but it hurts more every day and it is from standing and walking. I have been told by several people that the left leg is not straight. I cannot put my feet together without overlapping my knees. With my knees together my left leg is about 8-10 inches from the center. I keep saying something is not right, I have discussed this with the surgeon and the xrays for both knees look different. My PT’s can also see a difference. Swelling is minimal and I have good leg strength but cannot walk or stand without a lot of pain. I walk very poorly and I am trying very hard to work on gait.
Dear Jodie,
Seven weeks is a very short time after TKR surgery and certainly your knees are not fully rehabilitated. Your description of an angular deformity of your left knee with increasing pain while standing or walking is concerning. I would suggest you return to your surgeon and discuss your concerns and complaints and look for his or her advice. If you feel that “something is wrong” and these symptoms persist, I would consider seeking the advice of other orthopedic surgeons, preferably ones with a special interest and skill in revision surgery.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
i have had 2 tkr on LT knee in less than 2 years. By 2 different surgeons.i am having tracking problems. i dont know what to do. I had a tkr ,manipulation , patella put back on,adhesions removed and another tkr in august. Wasnt a month knee came loose . i am in a brace. I have iced down .i feel like i have been glued to this machine. i am so discouraged i am beside myself. please do you have any suggestion. no problem with incision healed well. I am now needing surgery again. any suggestons
Dear Mary,
Soft tissue imbalance can lead to these problems and often are secondary to components that are less than optimally positioned. It’s important that the underlying problem or problems are elucidated and then corrected. Unfortunately, obtaining an excellent result becomes more and more difficult with each surgery.
I would suggest discussing your concerns and frustrations with your surgeon and look for his or her advice. I also would consider further expert opinions. I have had success diagnosing imbalance by using the Verasence OrthoSensor, if one is made for the particular implant that you have.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello Dr.
I’m a fit and active 45 year old male who had tkr on my right knee 2/16/16. After the initial recovery, all was well and I felt great. I actually returned to sports (slow pitch competitive softball) in August without any issue. This past week I’ve had some pretty significant pain behind the knee cap area at certain points of flexion when walking. I get a painful twinge and the knee joint momentarily feels unstable. This just came on in the past week or so and although very active, I cannot recall a specific event that may have caused this. I have a follow up with my Dr 11/14 although I feel I may not make it that long. Any insight would be greatly appreciated.
Sincerely
Kevin W.
Dear Kevin,
Following up with your surgeon is most appropriate. Some patients develop nodules of fibrous tissue on the undersurface of their extensor mechanism, most typically where the quad tendon inserts into the patella. This nodular tissue can catch on the prosthesis as the joint moves. Most classically, it catches on the prosthetic notch of the femoral component during extension from a fully flexed posture. This is referred to as a patella clunk syndrome. It’s possible you are beginning to develop this. I suggest you discuss these concerns with your surgeon who will have specific recommendations.
I wish you well.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I had a tkr 16 months ago,and still, have terrible pain and not able to descend stairs properly or walk any distance without pain. I had random pitting edema in my knee and entire leg off and on and am still having swelling.I have felt as if I have had the flu for over a year and also had strange,random rashes.I was in PT for over six months and could not get good flexion. When I walk or bend my knee,it feels as if my knee isn’t tracking right.I went to my surgeon many times,complaining of pain and swelling and all he would do is pat my leg and said some people take longer to heal.I finally was able to get a second opinion after a year of pain,and that dr said the pain could be that he didn’t put a slider behind my own kneecap. Then he said my knee was ok and I had a 50% chance of surgery making it worse or better. He also examined my mri before surgery and said I did not need a tkr,as I wasn’t bone on bone.But,he also said,he wouldn’t do the surgery. Here I am six months later and now,my shoulder has a rotator cuff tear,have back and right foot pain and feel as if this surgery has DISABLED me and afraid I will end up in a wheelchair. I found a new ortho and they did a bone scan and it showed loosening. He now wants me to do a white cell progressive test to check for infection. He also thinks I need surgery for my shoulder.My knee never felt right from the get go and am wondering if this is a surgical mistake and malpractice? I am scared to death of more surgery. Please advise.
I had a TKR Jan. 8, 2014 and in more pain than ever before. I had had two previous surgeries on my knee in 1972, 1974 and they took my patella out with the one in 1974. They couldn’t save it due to Navy Doctor’s screwing up the first surgery. I had been seeing my ortho doctor on and off for about 10 years and finally had TKR on it with no patella replacement(.I have the greatest confidence in him and still do by the way. He’s as frustrated as I am) Muscles and tendons had to be rearranged due to the previous surgeries, let straightened and lots of bone spurs shaved off. I cannot straighten my leg without putting my other leg underneath it. I had 3 months of vigorous therapy and they can’t do any more. Now my Dr. says maybe I should have a patella put in / 3 months in a cast, straight leg with no guarantee that will solve the problem. My right hip needs to be done and I don’t know what to do. I have fallen several times, my leg just gives out on me; just not steady. I am 68 yr. old female, 5’1 and 107lbs. I did hair for 46 years so I stood on cement. Retired after the surgery; I couldn’t stand anymore. I just don’t know what to do or where to turn anymore….
Dear Colleen,
Your extensor mechanism is compromised. Many patients who have had their patellas removed still have an intact extensor mechanism and actually do quite well after TKR. The fact that you are unable to actively extend your leg, and it is resulting in falls, suggests that your extensor mechanism may not be complete or is disconnected. If that is the case, the operation your surgeon is recommending may be your best chance for success. It is typically performed using an allograft, which is tissue from someone who has died. It is a difficult and extensive procedure, one that almost no surgeons have extensive experience performing, and unfortunately one associated with a lot of complications. However, it still may be your best option.
If your arthritic hip is also causing a lot of problems, I’d consider having it replaced first. This is a much more predictable surgery with a lot of benefits. If you are going to proceed with allograft extensor reconstruction, I’d recommend you learn as much about it as you can beforehand.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hi Dr Leone
I had a TKR on the left leg, about 8 years ago, about a year later I had surgery on the same knee to revise what had been done the first time.
After the second surgery, about 1month, they did a manipulation because of the lack of ROM.
I do remember the Dr informing me that the parts used were not the correct size.
I am unable to get 90 degrees, and when walking, and I trip/stumble the pain in the knee is very very painful
Dear Clive,
It is doubtful that your range of motion will increase further this long after your last surgery. The cause of your tripping needs to be determined and understood. Are you tripping because your knee is stiff, and then when you trip, your knee becomes painful? Or, is the knee constantly painful and at times you also trip? It also is important to understand why you struggled to regain fuller flexion. Other aspects of you knee also must be evaluated including alignment, component sizing and position, as well as stability. Infection always must be considered.
If you feel disabled enough with your knee, then further revision must be considered. Depending on your answers to many of these questions, the risks of repeat revision must be weighed against the benefits.
My advice is to further discuss your ongoing difficulties with your surgeon. I think a second opinion may also be appropriate.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Had a TKR in March 2016. Recovery fairly normal, but now have a torn peroneus brevis tendon. Could it be connected to the TKR?
Dear Pat,
I am not aware of a direct relationship. It’s possible that your peroneus brevis tendon was compromised due to angular deformity from your arthritic knee. After TKR, which would have corrected your alignment, it’s possible that more stress was placed on the tendon resulting in a tear. Regardless, I hope you are doing well after TKR and now must address you difficulties with you ankle tendon.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello Dr. Leone,
It will be a year this December 14th that I had a total knee replacement and I am almost 66 years old.. I can straighten and bend my leg well when it’s not swollen. In May of this year my Sciatica flared up and my right hip is elevated. My flexer muscle is tight and the muscles on the outer and inner thigh bother me. I also am getting atrophy in the calve of my leg. In August I developed a small red spot on the side of my knee next to a bump that I had prior to the knee replacement. It has been cultured twice in the last three months and has come back negative. My surgeon referred me to a Dr. to get an epideral for my sciatic issues and this Dr. says he thinks I have CRPS which he has given me three nerve blocks. This helps for about 3 days. My balance seems good the moment after I have them and walk with a better stride. On the side of the knee and right below is where the redness develops. I went a month with no redness and now it’s back last week. It’s very spotty and goes away after about three days. During this time my leg gets so heavy I can’t lift it from a sitting position and can hardly stand on it. My surgeon wants to operate and take out the liner, clean and irrigate and take a tissue sample. I’m afraid that this will be to no avail. Not sure what to do and if you have any suggestions it would be appreciated.
Thank you!
Roxanna
Dear Roxanna,
If your surgeon is concerned there is underlying infection, in spite of you reporting two prior negative cultures, then I agree with his determination to rule out infection above all else. In my experience, the Synovasure test has been a powerful test on which I’ve learned to depend.
While it is possible that you have developed a CRPS (Complex Regional Pain Syndrome), which is characterized as a dysregulation of the central and autonomic nervous system, I would consider this a diagnosis of exclusion. First, I think other diagnoses that may be causing your problem should be considered and ruled out.
Without personally examining you, I question whether your right hip seems elevated secondary to a pelvic obliquity from underlying scoliosis. This is common. This is often associated with lumbar degenerative arthritis which can result in spinal stenosis and elicit the kind of symptoms you report in you right upper outer and inner thigh. Hip arthritis can also cause these symptoms. Symptoms to your ipsilateral knee need to be ruled out.
My advice is to discuss fully with you surgeon your concerns about having more surgery and what he or she thinks is really going on. Inquire if there is another way to learn if the knee really is infected short of exploring, debriding and changing the plastic. The Synovasure test has really helped me to clarify if an infection is present or not, even with negative cultures. Also, I would recommend discussing your chance of curing an infection, if one is present one year postop, with liner exchange and debridement.
If infection and other etiologies are ruled out and your physicians do think you’ve developed a CRPS, direction of care from your pain management physician will be very important.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Roxanna,
If your surgeon is concerned there is underlying infection, in spite of you reporting two prior negative cultures, then I agree with his determination to rule out infection above all else. In my experience, the Synovasure test has been a powerful test on which I’ve learned to depend.
While it is possible that you have developed a CRPS (Complex Regional Pain Syndrome), which is characterized as a dysregulation of the central and autonomic nervous system, I would consider this a diagnosis of exclusion. First, I think other diagnoses that may be causing your problem should be considered and ruled out.
Without personally examining you, I question whether your right hip seems elevated secondary to a pelvic obliquity from underlying scoliosis. This is common. This is often associated with lumbar degenerative arthritis which can result in spinal stenosis and elicit the kind of symptoms you report in you right upper outer and inner thigh. Hip arthritis can also cause these symptoms. Symptoms to your ipsilateral knee need to be ruled out.
My advice is to discuss fully with you surgeon your concerns about having more surgery and what he or she thinks is really going on. Inquire if there is another way to learn if the knee really is infected short of exploring, debriding and changing the plastic. The Synovasure test has really helped me to clarify if an infection is present or not, even with negative cultures. Also, I would recommend discussing your chance of curing an infection, if one is present one year postop, with liner exchange and debridement.
If infection and other etiologies are ruled out and your physicians do think you’ve developed a CRPS, direction of care from your pain management physician will be very important.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hi. I had TKR & am 3 mo. Post op. Have had major complications with pain & instability. D-dimer of 779. HBP since surgery going to 165/120. Inability to walk more than a few minutes. Knee buckles. Chest CT clear & bilateral LE Doppler clear. Still on pain meds. PT says my recovery is not normal as any weight causes severe pain. My surgeon initially tried to say it was all in my head. He does not return calls. Op rpt is only 1 page long & very inarticulate. Deformity of my inner thigh since surgery. No other surgeon will touch me for at least a year post op. Can’t get back to normal life or enjoy anything. Can you guide me to someone in NY who can help? NY is where I live.
Dear Sheri,
It remains my policy not to recommend specific surgeons or institutes in this format. Your postop course does sound very unusual and difficult. You describe postop medical complications as well as weakness, pain and deformity associated with your TKR. As a general rule, it is best to wait a year postop before concluding a TKR needs further surgery. There are of course exceptions to the general rule. There are situations when it becomes apparent that a problem is not getting better or is even getting worse and cannot possibly improve without intervention. If you remain this disabled, then I would recommend that you seek further opinions from orthopedic surgeons who specialize in TKR and revision. Fortunately, you live in a part of the world where there are many capable orthopedic surgeons.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Sheri,
It remains my policy not to recommend specific surgeons or institutes in this format. Your postop course does sound very unusual and difficult. You describe postop medical complications as well as weakness, pain and deformity associated with your TKR. As a general rule, it is best to wait a year postop before concluding a TKR needs further surgery. There are of course exceptions to the general rule. There are situations when it becomes apparent that a problem is not getting better or is even getting worse and cannot possibly improve without intervention. If you remain this disabled, then I would recommend that you seek further opinions from orthopedic surgeons who specialize in TKR and revision. Fortunately, you live in a part of the world where there are many capable orthopedic surgeons.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hi
I live in South Georgia. I had a TKR in June 2013. I did great with it. I was faithful to my therapy. Today I still do my exercises. My knee is killing me. For the first year everything was good even though I did experience a little pain and numbness. Now it is still numb and it feels as if it’s going to go through my skin. The pain is unreal. It swells, and I ice it. Does it help? Yes for about an hour. I find that I can’t walk or stand for more than about 45 minutes at the time. This pain makes me ill. It hurts like hell most of the time. Now I’m needing the other one done but keep putting it off because I’m not happy with the one I had replaced. My surgeon is top notch down here. I am the only one that’s having these kind of issues.
Ohhh please tell me what’s going on with this thing
Dear Kaye,
It appears that with time, your symptoms have become worse. During your first year after surgery you were satisfied despite “a little pain and numbness,” symptoms have escalated and are now disabling. This may be a clue to the underlying problem. The supportive soft tissues that support the knee are not balanced and / or the components not optimally related to each other (congruency) in some individuals who have undergone TKR will present similar symptoms. This is actually not uncommon and I often refer to this group of patients as “looks good but feels bad” because their X-rays often look acceptable, their incision healed nicely, they can walk a short distance without a limp but are miserable with continued activity. I have had success treating in a number of patients using kinematic sensor technology to help me pin point the mechanical problem(s) and then address surgically to correct.
I would recommend that you discuss your concerns with your doctor. If this individual is not able to help you, I would recommend you seek out other opinions from orthopedic surgeons with a special interest and expertise in TKR and revisions to help you solve your problem.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Kaye,
It appears that with time, your symptoms have become worse. During your first year after surgery you were satisfied despite “a little pain and numbness,” symptoms have escalated and are now disabling. This may be a clue to the underlying problem. The supportive soft tissues that support the knee are not balanced and / or the components not optimally related to each other (congruency) in some individuals who have undergone TKR will present similar symptoms. This is actually not uncommon and I often refer to this group of patients as “looks good but feels bad” because their X-rays often look acceptable, their incision healed nicely, they can walk a short distance without a limp but are miserable with continued activity. I have had success treating in a number of patients using kinematic sensor technology to help me pin point the mechanical problem(s) and then address surgically to correct.
I would recommend that you discuss your concerns with your doctor. If this individual is not able to help you, I would recommend you seek out other opinions from orthopedic surgeons with a special interest and expertise in TKR and revisions to help you solve your problem.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone,
Thank you for taking the time to address everyone’s issues. I’m a 66 year old male who had ligament surgery on my left knee at age 23. Over time the cartilage wore out and I had a TKR in January of this year. For the first 6 months things progressed slowly but surely. Since later in July things have been going the wrong way. I’ve always had a clicking on occasion with the new knee but was told that’s not uncommon. My chief problem is a severe pain in the back of my knee ( even at rest) that shoots down to my heel. I saw the original surgeon in August & October. He took more x-rays & ordered blood tests to rule out infection. Having lost confidence in the original surgeon I went for a second opinion. The new Dr. did a very through exam ( including reviewing all X-rays) and ordered a bone scan which was inconclusive. He then gave me a Cortisone shot which worked like a miracle. I know this is only a temporary fix and when it wears off I’ll be back to square one. Based on my history do you have any opinion as to what might be wrong?
Best Regards,
Mark Halkin
Dear Mark,
It’s concerning that you are experiencing increasing symptoms after the first six months. Typically, I would expect your symptoms to be improving or at least stabilizing at that point. The fact that an intra-articular injection relieved your symptoms, strongly indicates that the pain is being generated by a problem within the knee capsule. Soft tissue instability and/or less than optimal rotation between the femur and tibia can cause pain. A prosthesis that is extending beyond the peripheral margin of bone can also potentially irritate overlying tissue. I’ve cared for a number of individuals who developed posterior knee pain after TKR from the tibial component over hanging the cut surface of the tibial and irritating the popliteus tendon.
I would not be quick to place more cortisone into the knee if your symptoms return. Ultimately if your symptoms do return, then you’ll most likely require more surgery to resolve it. Surgery must address the underlying problem and correct it.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Mark,
I’m concerned that you knee is getting worse with time not better. It’s interesting that you were improving over the first six months and then began to decline. I have replaced knees in a number of patients who had major ligamentous reconstructions done many years prior. Original anatomic soft tissue structures were re-positioned to give the knee support after injury.
So years later when a TKR is done, an attempt is made to balance the surrounding supportive soft tissue sleeve. But the surgeon is now releasing/balancing non-anatomic structures that are critical to support normal movement and stability of the new prosthetic knee. In my experience, these non-anatomic soft tissues often weaken or stretch out after initially doing well, at which point the knee can become unstable and painful. Repair may require implanting a prosthesis with more internal constrained which does not depending on the soft tissues to the same degree.
The cortisone injection suggests the problem is within the knee joint capsule and not extra-capsular or referred from another source.
Mark, there are many reasons why your knee may hurt. What I have outline is one possible reason. Unfortunately, if symptoms return and you remain disabled, then you need to discuss your problem with your surgeon and look for their recommendations to treat you. It’s possible that a revision or re-do surgery will be necessary.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Mark,
I’m concerned that your knee is getting worse with time not better. It’s interesting that you were improving over the first six months and then began to decline. I have replaced knees in a number of patients who had major ligamentous reconstructions done many years prior. Original anatomic soft tissue structures were re-positioned to give the knee support after injury.
So years later when a TKR is done, an attempt is made to balance the surrounding supportive soft tissue sleeve. But the surgeon is now releasing/balancing non-anatomic structures that are critical to support normal movement and stability of the new prosthetic knee. In my experience, these non-anatomic soft tissues often weaken or stretch out after initially doing well, at which point the knee can become unstable and painful. Repair may require implanting a prosthesis with more internal constrain and does not depending on the soft tissues to the same degree.
The cortisone injection suggests the problem is within the knee joint capsule and not extra-capsular or referred from another source.
Mark, there are many reasons why your knee may hurt. What I have outline is one possible reason. Unfortunately, if symptoms return and you remain disabled, then you need to discuss your problem with your surgeon and look for their recommendations to treat you. It’s possible that a revision or re-do surgery will be necessary.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.