Joint Replacement Surgery for Osteoarthritis Q&A
As comments and very detailed questions from readers continue to be posted on my blog, it occurred to me that it was time to do a series of Q&A posts that talk about joints and why they deteriorate, as well as what treatments and surgeries are available today to get people back on their feet and enjoying a pain-free lifestyle. This first post addresses the most common cause of joint deterioration: osteoarthritis. Simply put, osteoarthritis occurs when hyaline cartilage, which is the specialized tissue that covers the ends of the bones in a joint, is damaged or worn away to the point of “bone on bone” friction. Hyaline cartilage is not self-repairing and, when damaged, results in pain and diminished movement, progressively disrupting one’s quality of everyday life. As the osteoarthritic condition progresses, it can lead to immobility and one’s loss of independence. Below are a few of the most common questions regarding osteoarthritis and joint replacement surgery:
What is joint replacement surgery for osteoarthritis?
Total joint replacement surgery is a procedure where the diseased cartilage and bone of the joint are surgically replaced with artificial materials.
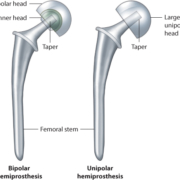
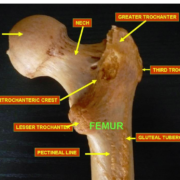
The total hip replacement prosthesis consists of a ball which is made of metal or ceramic, which is held in a precise position by a metal stem. The stem is inserted down the marrow cavity of the femur. The ball is inserted into the new socket which consists of a liner with special wear characteristics and which is supported by a titanium shell placed next to living bone so that bone grows into it.
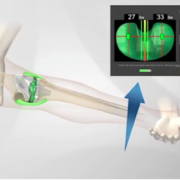
When a total knee replacement is performed, the bone and cartilage on the end of the thigh bone (femur), top of the shin bone (tibia) and the underneath surface of the patella or knee cap are replaced with metal and plastic parts so as the joint moves the plastic slides against the metal parts and friction is minimized. The “art” is to perfectly realign the limb and balance the supportive tissue so the knee feels natural.
One way the knee is different than the hip is that the knee has three compartments rather than one. Depending on the location and severity of the arthritic process and the deformity, many times only one or possibly two of the compartments requires resurfacing, which is called a partial knee replacement. This has the advantage of a much smaller surgical dissection and faster recovery time.
When is it time for joint replacement surgery for osteoarthritis?
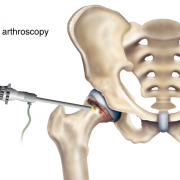
Osteoarthritis is one of the most common causes of hip and knee deterioration and destruction. If you are experiencing pain or disability that is interfering with your ability to be independent or active, it’s time to have a conversation with your doctor followed by a thorough examination. When all conservative treatments methods have been exhausted such as NSAIDs, other pain modifying medicines, therapy, activity modification, modalities like ice or heat and possibly injections or even arthroscopy, and your quality of life is severely affected, joint replacement surgery may be the next step.
Is Joint replacement surgery for osteoarthritis common?
Total hip replacement surgery has been one of the most successful surgeries ever developed. In fact, total hip replacement and cataract surgery are considered by many as the two surgeries that during the last century have had the greatest effect on improving quality of life. The latest statistics gathered by the Centers for Disease Control and Prevention (CDC) show that some 327,000 hip replacements are performed annually in the U.S. That number is roughly double for knee replacements. The number of total hips is predicted to increase to nearly 600,000 in the U.S. alone by the year 2030. Although both hip and knee replacements traditionally were reserved for the elderly, today patients aged 45-54 are a much-faster growing demographic. It is predicted that nearly 3.4 million knee replacements will be performed in the U.S. by 2040.
How does joint replacement surgery ease osteoarthritis symptoms?
Today, people no longer are willing to endure living with debilitating pain and disability or give up active lives when joint replacement is a safe and viable alternative. Some attribute this shift in mindset to the baby boomer generation because people are living and remaining active longer both in the workplace and with social and sports activities. And, while some activities simply are not appropriate for patients who have had a hip or knee replacement, we keep rewriting the rules because of patients who are succeeding with remarkably pain-free, active lifestyles. I allow and even encourage my patients to participate in activities that the surgical community never would have sanctioned in years prior, including singles tennis, downhill skiing and ice hockey, if this is their passion.
Joint replacement very predictably relieves the pain of osteoarthritis by replacing the ends of the bones that make up the joint with artificial parts so the bones are no longer rubbing or grinding together. On an X-ray we see “bone on bone” deformity. After joint replacement, secondary “reactive” changes such as synovitis (lining of the joint is inflamed) and joint effusions (increase fluid in the joint) then also quiet down. Joint function also normalizes with the reconstruction of normal body mechanics and alignment and because the joint is no longer painful. When a partial knee replacement is done, the hope is by realigning the limb and rebalancing the supportive soft tissue sleeve, the progressive destruction of the knee with be halted and the remaining compartments that were not replaced will remain healthy.
Please read Dr. Leone’s BLog on the latest hip technique called the SPAIRE Approach. Click here.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.