Hip and Knee Q&A: Common Questions about Joint Pain, Pain Management and Treatment
In the second of a three-part Q&A series about joints, here are some of the most common questions patients at The Leone Center for Orthopedic Care ask about hips and knees. In a previous blog, I discussed arthritic joints. The third blog of the series will detail common questions specifically about surgery.
What causes hip and knee pain?
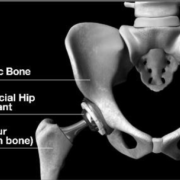
Hyaline cartilage is the super specialized cartilage that covers the ends of the bones that meet to form a joint. This specialized cartilage acts to decrease friction and distribute the weight bearing forces. If the cartilage is destroyed or diseased and the bones are no longer covered, then the bones rub together. This condition is referred to as bone-on-bone and results in nerve endings within the bones to be stimulated and exposed resulting in pain.
Synovial tissue lines the joints and produces synovial fluid that also helps lubricate and nurture the hyaline cartilage. When there is a problem within the joint, synovial tissue often responds by producing more fluid than usual. It is easier to see in the knee than the hip but this increase in fluid can distend the surrounding capsule and cause pain. This increase of synovial fluid, called an effusion, has a denser concentration of hydrolytic enzymes that also further injure that cartilage.
If a mechanical problem has developed within the hip or knee, it may result in abnormal motion or instability which can also cause unintended and unnatural movement and result in pain. There also are pain receptors in supportive ligaments (i.e., medial and lateral collateral and cruciate ligaments) that in an arthritic joint become stimulated as the joint becomes more compromised, thus contributing to the pain someone experiences.
If a person has undergone any prior surgery including a joint replacement, infection must be considered when trying to establish the etiology of pain. Also, a mechanical problem such as component loosening or a biologic problem such as an allergic hypersensitivity to the prosthesis also can result in pain.
How can I prevent knee and hip pain which results from sitting all day?
Many individuals who develop knee or hip arthritis struggle with prolonged sitting or finding a comfortable position once seated. Classically, they also experience “startup” pain when they first arise from the seated position and with their first several steps.
Conservative measures to treat arthritis pain exacerbated from sitting include NSAIDs, stretching and strengthening exercises, limiting the time you stay seated and trying different chairs at different heights. Some people work off special “standing” or “kneeling” desks to mitigate this. Understanding the etiology of the pain will help create the proper treatment plan.
What are some causes of hip and knee pain during jogging?
First, do not buy into “no pain, no gain.” Pain is a warning signal from the body of a nocuous or detrimental stimulus or condition. Pain has evolved to protect our bodies.
If jogging results in hip pain, then I suggest stopping until the source of the pain is understood. If a workup does reveal that there is a particular problem with the hip or knee joint or even another source such as the lower back, then that problem needs to be treated and resolved before jogging is resumed. If the workup reveals an intra-articular problem with the hip such as osteoarthritis or dysplasia, then jogging should be stopped altogether because to continue would hasten the demise of the joint. Finding another way to exercise, which imparts less impact to the joint such as swimming or biking, would be more appropriate.
If the workup does not reveal a significant mechanical problem with the joint, then change the jogging conditions: the terrain (jog on grass rather than the road) or shoe type. Optimal pre-jog stretching and other conditioning also should be an habitual part of the routine.
Could there be another cause for my hip or knee pain?
Identifying the etiology of both hip and knee pain is not always easy or straightforward, because pain perceived in one location potentially can be originating from another location or source. We call this referred pain.
Many times what people perceive as hip pain is actually pain that is being “referred” from another source such as the lower back. Classically, people will complain of deep buttock pain thinking it’s from the hip when it is actually being caused by irritated lumbar nerve roots from the lower back. Additionally, knee pain also can be “referred” from a problem originating in the hip.
Someone who has a hip or knee replacement that is not functioning optimally or is infected also can experience pain.
In addition, the origin of hip pain needs to be clearly understood before it can be treated, i.e., is the pain being caused by a problem within the hip joint capsule (intra-articular), or from an outside (extra-articular) source? Examples of an intra-articular problem would include osteoarthritis or rheumatoid arthritis that destroys the joint’s articular cartilage. Examples an extra-articular problem include a greater trochanteric bursitis or iliopsoas tendonitis.
An intra-pelvic source such as an ovarian cyst or hernia must also be considered.
How can I tell if the pain is from my back or a bad hip?
Sometimes, distinguishing between hip or back pain is difficult because the patient is feeling pain from both sources. Often, a person who develops an arthritic hip has the same genetic predisposition to develop an arthritic back, and a symptomatic hip can cause back pain secondary to awkward body mechanics and/or a limp even if he or she doesn’t have significant back pathology. Many individuals with significant back pathology experience sciatic pain in the hip and leg caused by existing spinal nerve roots which are being squeezed or irritated. The distinction usually can be made with a careful clinical history and physical exam. Good imagining such as X-rays or an MRI scan also is important. Occasionally a pain injection test or epidural injection will also help distinguish the source.
What exercises can help relieve joint pain?
It depends what is causing the pain. In general, keeping the muscles that control the hip or knee strong, while optimizing flexibility, helps to preserve function and mobility. I encourage pool walking, swimming, biking, light weights and flexibility training, core strengthening, and weight loss, if indicated.
How do I know if joint surgery is right for me?
The following signs might help you determine if the time is right to have a thorough conversation with your doctor to explore all of the treatment options, including joint replacement surgery:
• If pain keeps you awake at night or you wake up from sleep.
• If pain limits your ability to perform typical daily activities such as walking, climbing stairs, or getting up and down from a sitting position and in and out of your car.
• If pain limits leisure activities such as walking, exercising, dancing, golf, tennis, dancing, traveling or even shopping.
• You have tried other less-invasive treatments for a suggested period of time, such as exercise, physical therapy, a brace, anti-inflammatory medicines, or injections.
• If you are experiencing total frustration that you are losing your quality of life due to impaired mobility or pain.
• You are developing a progressive loss of motion or progressive deformity
What problems might occur after joint replacement surgery?
Both hip and knee replacement surgical techniques and the prostheses we implant have greatly advanced, allowing surgeons to perform less-invasive and more precise and more predicable procedures. Our expectation is that these prosthetic joints will preform for many more years than earlier generation joint replacements. Patients also are getting well much faster, partially because they are experiencing so much less pain after their surgeries, than just a few short years ago. This is due to improved surgical techniques, better anesthetic medicines and better pain control after the procedure. Meticulous soft-tissue handling to minimize trauma to tissues is critically important as well as optimum prosthesis placement. It is important for your surgeon, as well as the hospital, to have significant experience and a proven track record with these surgeries.
The risk of infection remains a constant concern and we are very proud of our track record at The Leone Center for Orthopedic Care. It requires a constant “hypervidulance” and awareness. The incidence of infection is related to the surgical technque, gentle soft tissue handling and the experience of the surgical team. Also, if a patient has pre-existing conditions such as obseity, diabetes, heart conditions or other medical problems, then these conditions must be fully studied and optimized prior to surgery so they can be managed fully post-operatively.
Can joint replacement be done with minimally invasive surgery?
I think every surgery should be done using as minimally invasive a technique as possible, while emphasizing precise component positioning and soft tissue balance. There are times when making a larger incision or releasing more soft tissue is “less invasive” because if it were not done, tissues would be torn and stretched causing more trauma and bleeding. In every operation I do, I emphasize being gentle and precise. In my experience these are the patients who have less pain, get well the fastest and ultimately have the best results. They also are very grateful.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.