Q&A: Total hip replacement, mini-posterior vs. direct anterior surgical approaches

How invasive is the mini-posterior approach?
This approach involves separating the muscle fibers of the large buttock muscle (gluteus maximus) located at the side and the back of the hip. Because only the “distal” or bottom third of the muscle fibers are separated, not cut, the nerve pathways are not disturbed and the muscle is not injured. The “proximal” or upper short external rotator muscles are released from their attachment into the upper femur. The hip joint capsule is opened “posteriorly” or in back. These structures including the hip joint capsule are repaired after implanting the total hip components Special tables and imaging equipment is not required when performing a mini posterior approach.
What are some of the advantages of the mini-posterior?
Most consider the posterior approach a more straightforward approach than the anterior approach so there are less complications. Typically, there is less bleeding associated with the mini-posterior approach, so the need for blood transfusion after surgery is less. Because femoral exposure is better, there is a lesser risk of femoral fracture, especially when operating on osteoporotic bone. Because femoral exposure is better, it encourages the surgeon to choose the most appropriate femoral implant (which may not be the shortest or the non-cemented stem) rather than the one that is easiest to implant.
Very important, if the exposure of the hip joint when performing the surgery proves more difficult than anticipated (and this happens) or should a femoral or acetabular fracture occur, the mini-posterior approach is easily extended to improve the exposure to address and fix the problem. The risk of nerve injury is also less with the mini-posterior approach vs. the anterior approach.
What are some of the disadvantages of the mini-posterior?
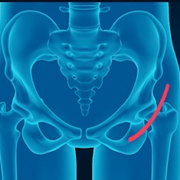
There is an increased incidence of posterior dislocation because the posterior hip joint capsule is opened and the upper short external rotators are released from their femoral attachment, until these tissues heal. Patients who had a THR using a “classic” standard posterior approach were taught “hip precautions”. These were positions that patients were instructed not to put their leg in. Many folks were never given a timeline when they could stop worrying about it. They were taught not to bring their knee higher than their hip (greater than 90º), not to cross the mid line with their leg (adduct) and not to internally rotate the leg (avoid having knee and foot twisted in). All of these positions stretch the posterior capsule and repaired structures and potentially could lead to dislocation. However, as of 2020 Dr. Leone is using the latest hip technique called the SPAIRE technique where patients no longer have hip precautions after surgery. For details please read his blog on this technique.
Using a mini-posterior approach and modern techniques to close the capsule and short external rotators, combined with modern prosthesis with larger head sizes, the risk of dislocation is extremely small and many surgeons now don’t recommend any hip precautions.
The SPAIRE Technique: this is the technique I have been using to care for my patients since 2020. One of the greatest advantages is there are no restrictions or precautions after surgery. Read the latest article here.
How invasive is the direct anterior approach?
It involves dissecting between two main muscles located at the front of the hip and upper thigh. The hip joint capsule is opened “anteriorly” or in front. Often, part of the quadriceps attachment into the capsule and pelvis is released to improve exposure. Some surgeons use special tables that facilitate femoral exposure by applying traction on the leg as it’s moved into various positions. Care must be exercised not to apply too much traction which can damage soft tissues, nerves and the ankle.
Are there any advantages to the direct anterior approach?
I think the biggest advantage to the anterior approach is there are no positional restrictions or “hip precautions” immediately after surgery. Because the hip joint capsule is opened anteriorly (in front) there is a lesser incidence of posterior (in the back) dislocation. On the other hand, there may be a slightly increased incidence of anterior dislocation. Clinically, patient is not restricted from sitting on a low seat or bending to pick something off the floor without keeping their leg back, very soon after their surgery.
The literature reports a slightly smaller dislocation rate after an anterior approach vs. the “classical” posterior approach. I think the incidence of dislocation with both approaches is surgeon and technique dependent.
Because the patient is lying on their back during an anterior approach, it facilitates using a fluoroscope or moving x-ray throughout the procedure. This does expose the patient to more radiation but can help with component positioning, sizing and leg length measurements.
What are the disadvantages of the direct anterior approach?
There is an increased incidence of nerve injury after the anterior approach. The nerve most commonly injured is the lateral femoral cutaneous nerve which provides sensation to the anterolateral thigh (or part of the front and outside of the thigh). The incidence of sciatic nerve injury after an anterior approach is less than with the posterior approach. When is does occur following an anterior approach, it’s most likely caused by traction from the table used to gain exposure. The intended interval between the front thigh muscles can be difficult to recognize and there has been an associated increase in injury to the femoral nerve or vessels.
There is an increased incidence of femoral fractures, especially in osteoporotic bone. If the fracture occurs intraoperatively, extending the incision to expose the fracture to fix it can be very difficult and may require an additional incision. Because femoral exposure is difficult, many of these fractures are not appreciated at time of surgery, but discovered a week or two later with femoral stem subsidence (the stem moves down towards the knee and the fracture then opens up). A second trip to the operating room is then necessary.
Because femoral exposure is more difficult, shorter, press-fit stems are being implanted because they’re easier to implant. Many times these may not be the optimal stems for that particular patient but are chosen because they are easier to implant through the anterior approach. That patient’s anatomy may be better suited for a longer stem or one implanted with bone cement. Many of these short stems have been designed specifically to make them easier to insert anteriorly. Many have very short track records. Historically, short press-fit stems have not done well. Our hope is that these will.
I see a number of patients in my practice who come to me after already having undergone a THR via the anterior approach. Frequently, I see the femoral stem is not optimally aligned down the upper femur but rather implanted on an angle resulting in the end of the stem touching the inside of the femoral cortex. Sometimes this causes a stress reaction and pain. Once again, this is occurring because femoral exposure is poor and it is more difficult to optimally align a short stem which is being chosen because they are easier to implant.
The anterior approach has more intraoperative bleeding than the mini-posterior approach. This can result in an increased need for blood transfusion after surgery. The type of anesthesia and the specific individual doing the surgery are critical factors associated with blood loss.
What type of surgeon or hospital setting should a patient look for?
Experience cannot be overemphasized. Choose an orthopedic surgeon with whom you are comfortable and treats you and not your x-rays. It’s also important to choose a hospital with a proven track record and reputation for excellence in joint replacement surgery.
A priority for anyone considering hip replacement surgery is to find a doctor you trust and who has an excellent reputation for performing THR. You want a surgeon who will spend the time to make a clear diagnosis and develop a plan that will meet your individual needs and goals. It’s also critically important that your doctor has a support team that is welcoming, nurturing and knowledgeable.
In your experience, which approach would you recommend?
The most important decision you must make is choosing the surgeon who will take care of you. While I think the approach is one important variable, recognize it’s one of many, many decisions that must be made for the end result and the experience to be as perfect as they can be. The individual who is actually doing the surgery is more important than the approach he or she chooses to use.
Although I am trained in both approaches and have trained surgeons in both approaches, I have stopped using the anterior approach because I saw my patients get well faster, bleed less, and have a more predictable result when I performed the surgery using the SPAIRE Technique. I’ve concluded that perceived benefits do not outweigh the risks with the anterior approach, especially when I can achieve the same or more using the mini-posterior.
If you do enough surgery, complications happen. Critical for me is always knowing what the next step is and being able to execute it, should a complication occur. I think it’s important that an incision and dissection can be extended (made longer) if necessary. This is easily done when using the SPAIRE Technique, this is not the case when using an anterior approach.
My recommendation is to choose your surgeon, not the approach, then trust that individual to take care of you.
When a patient is considering hip surgery, what is most important?
Therefore, as of 2020 I am using the latest hip technique called the SPAIRE technique where patients have no hip restrictions after surgery. For details please read his blog on this technique.
To stay focused on the outcome: excellent results both short and long-term with minimal risk of injury or complication. Don’t lose sight of the real goal, to have a perfectly positioned reconstructed hip that is stable, balanced and has the best possible chance of lasting more than twenty years. The most important decision a patient can make is choosing the doctor who will perform their surgery.
Check out Dr. Leone’s Patient Testimonials. These grateful patients make it all worthwhile.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.