The Pros and Cons of Two Approaches to Hip Replacement: Mini-Posterior and Direct Anterior
In my last blog post, I discussed minimally invasive surgery with regard to hip replacement. While new techniques, instruments and prostheses have been developed specifically for minimally invasive surgeries, there are many well-established approaches to hip replacement. Two which are receiving the most attention are the traditional posterior approach and the direct anterior approach. I would like to share my experience with both procedures.
The traditional posterior approach is the most commonly used in the United States and throughout the world (about 70 percent). The majority of teaching institutions in the United States continue to instruct as well as perform the traditional posterior as their primary approach. The mini posterior approach essentially is the same as the traditional posterior, however a smaller incision is made and less soft tissue is exposed. Very important with both the traditional posterior and the mini-posterior approaches, if the surgeon is not able to visualize critical structure adequately, or if a problem were to arise such as a fracture, then either approach can easily be adjusted.
Over the last six years, I have performed more than 2000 primary or first-time total hip replacements using the mini-posterior approach and I am aware of only one patient who dislocated his hip because he fell down stairs. His hip ball was put back in the socket and he has done beautifully since.
Mini-Posterior Approach
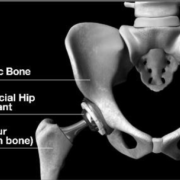
The mini-posterior approach involves separating the muscle fibers of the large buttock muscle located at the side and the back of the hip. Because the muscle fibers are separated, not cut, the nerve path is not disturbed and the muscle is not injured. Advantages of this procedure include:
- The mini-posterior is considered a more straightforward approach then the anterior, resulting in lesser complication rates.
- There is significantly less bleeding with the mini-posterior approach, notably reducing the necessity of a blood transfusion after the surgery.
- In my experience, there is a faster and more-consistent recovery with the mini-posterior.
- I have seen a number of patients who were reconstructed with the anterior approach who developed painful anterior scarring after the procedure. This then becomes a very difficult problem to solve.
- Because the mini-posterior is more straightforward, many surgeons think it provides an increased margin of safety for the patient, because the incision can easily be extended if exposure is poor, or if a fracture occurs.
- Because of the straightforward exposure of the femur, there is less risk of femoral fracture or poor implant positioning. Should one of these events occur during a mini-posterior procedure, they are easier to recognize and correct.
- Because visualizing the femur is easier, an experienced surgeon can choose the most appropriate femoral implant rather than just the one that is easiest to implant, taking into account the patient’s bone quality, activity level and age.
- There is less risk of neurological injury.
- No special surgical equipment is required when performing a mini posterior.
- As of 2020 only Dr. Leone is using the latest hip technique called the SPAIRE technique where patients no longer have hip precautions after surgery.
Direct Anterior Approach
The direct anterior approach involves dissecting between the natural intervals of the two main muscles located at the front of the hip and upper thigh. Because the patient is lying on his back, it facilitates using a fluoroscope or moving x-ray throughout the procedure. This does expose the patient to more radiation but can help with component positioning and sizing. There tends to be a lesser incidence of posterior instability with the anterior approach. On the other hand, there may be a slightly increased incidence of anterior instability. Along these same lines, there is a smaller incidence of sciatic nerve injury with the anterior approach but an increased incidence of femoral nerve injury. This is because the nerve is located in front of the hip. Also, because technically it is easier, many patients are being reconstructed with very short stems which are press fit into the bone during an anterior approach. These stems are a new design, and therefore do not have an established track record. Historically short press fit stems have not done well. The hope is that these new designs will, but time will tell.
Disadvantages of the anterior approach include:
- The nerve which supplies sensation to the front and side of the thigh is vulnerable.
- The intended interval between the front thigh muscles can be difficult to recognize and there has been an associated increase in injury to the femoral nerve or vessels.
- The physical build of some patients increases the difficulty. This is particularly true if the person is overweight, has very muscular thighs or is short.
- It also is more difficult for patients with some patterns of arthritis such as “protrusio,” which causes the worn out ball to migrate inward rather than upward into the socket.
- As noted above, because the femur is difficult to visualize, component positioning, sizing, and stability are more likely to be compromised. Also, the choice of femoral stem is more likely to be influenced by the approach and not the person’s anatomy and hip mechanics.
- More soft tissue trauma can result do to this increased difficulty in exposure and then gaining more exposure if necessary. Occasionally this even requires making a second, separate incision.
Although I am trained in both approaches and have trained surgeons in both approaches, I have stopped using the anterior approach because I saw my patients get well faster, bleed less, and have a more predictable result when I performed the surgery using a mini-posterior approach. I’ve come to the conclusion that perceived benefits do not outweigh the risks with the anterior approach, especially when I can achieve the same or more using the mini-posterior.
It is so important to stay focused on the outcome of your hip replacement surgery: excellent results both short- and long-term with minimal risk of injury or complication, and not lose sight of the real goal, which is to create a perfectly positioned reconstructed hip that is stable, balanced and has the best possible chance of lasting more than twenty years.
Ultimately, you and your surgeon should discuss all procedures and technologies available and then trust that your surgeon will choose the best course of treatment and surgical procedure for you.
I know the most important decision you will make is choosing the doctor who will perform your surgery. You should not proceed unless you know in your heart that you will be taken care of in a manner that has the best chance of giving you as perfect a result as possible.
As of 2020 only Dr. Leone is using the latest hip technique called the SPAIRE technique where patients no longer have hip precautions after surgery.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.







Thank you for this! My husband, who is only 35, has to consider a THA in the near future and I’m very torn over which approach as the surgeon we really like dos a posterior but I am concerned about dislocation rates in posterior vs anterior. But this blog was a nice nudge toward the posterior. Like you said, consistent outcome is important and this surgeon is excellent and I have great faith in him (I’m a physical therapist and see his patients post-op so get to see the, at least short term, results myself). We have an appointment today to discuss the plan of action.
Had a total hip replacement aug 2013. Woke up with
No feeling in my leg and no movement
Above the ankle to the thigh.Had to use leg brace to
Remain upright . 4 mts later am using
Walker to get around. Having physio
2 x week. Very slow recovery. Also had
Femor fracture. Nobody wanted to talk
About this injury to me. . Hospitsl staff
Would not make eye contact. Very strange
Behavior. If was 3 weeks after discharge
That I knew this recovery may take 1-2
Years!! Felt very uninformed and left
In the dark to find out about this myself
Tina, which procedure did you have? Posterior, mini posterior or anterior?
Very sorry to hear of the difficulties you experienced! Have you recovered by now? Which approach did the doctor take? Posterior or Anterior?
I had the mini-posterior at MGH hospital. Stay was 2.5 days. Tossed the cane at three weeks and went back to work. I am 5 weeks out and have been doing beautifully! Still going to rehab to reduce stiffness and increase strength but I am in better shape now than before surgery
Who was your surgeon at the MGH?
Thank you for this information. I am having the mini posterior done in June and my surgeon gave me the pros & cons of both. He is well known as a top doc for 20 yrs & I was persuaded because the mini posterior has less chance of nerve damage & the surgeon has more options for types of spikes, which your article explains well. Even though I was positive I wanted this method done, I was still questioning my decision. Your article has made it clear I made the correct decision, especially since my daughter had nerve damage from an operation years ago.
I am scheduled for total hip replacement in about 3 weeks, and none of these procedures/options were discussed with me………….the surgeon just said that it was a risky surgery and he could not guarantee anything!
Since I previously had both knees replaced (by another surgeon) about 5 years ago and still have problems with the knees i.e. crackling noise/pain, cannot bend them or kneel in church or get on the floor to do exercises, I am very afraid to ending up in a wheelchair or having to use a walker the rest of my life………….I am a very active 65 year old, and very, very worried about the hip surgery. Also, the surgeon said that I would end up having one leg shorter than the other… is this true? ………I am already limping when walking and was hoping that the limp would disappear after the hip surgery.
Also, I am diabetic and have had two organ transplants and am extremely worried about infections, etc. My question is: should I just tolerate the pain and limp, or take a chance with the hip replacement. Can you suggest any pain medication that would not interfere with anti rejection drugs?
Dear Annette,
I think it’s vitally important that you go into surgery truly believing in your heart that you are going to do well, and that you are with the best surgeon and team who will help you. Having diabetes and two organ transplants does significantly increase your risk for post-op infection as well as other complications. I would look at the published track record of the hospital where the surgery is scheduled to be sure its performance record is good and its incidence of infection is low. In my experience, most patients who undergo a total hip replacement don’t limp after their surgery and most feel their legs are the same length. There always are conditions or circumstances that may predispose one to limp or feel as if their legs are not the same length after surgery, but in my experience this is the exception. Most importantly, I would meet with your surgeon and discuss all of these concerns. By far the most important variable is the doctor who is doing your surgery and managing your post-op care.
No, I would not tolerate the pain and immobility, if there is a reasonable way to relieve it. Total hip replacement is one of the most successful operations ever developed and is a remarkably predictable way to relieve pain from arthritic conditions. If your surgeon has recommended surgery, I assume you’re no longer getting adequate relief of pain or able to remain active with conservative measures. I would research and find the physician and hospital that will give you the best chance of doing well. Yes, you do have increase risks. Yes, you can do very well.
William A. Leone
I had an anterior right hip replacement in late 2010, I was 72. Had horrible groin pain issues and opted for the antior, I knew of nothing else as I consulted with a surgeon who was trained in anterior.
I had good results into 5th month post op and then everything went downhill.
I deal with major nerve damage on front of thigh, almost whole thigh. Iliotibial (IT band) damage, had 2 months of ART release work on this issue.
It’s been a nightmare for me going into 4 yrs post op soon.
Granted I do deal with lower back OA and right knee OA and now all worse and now foot/ankle mess, all on right hip side.
I was so against doing this surgery but groin pain was very bad and crushed bone in the groin. No groin pain NOW….but all the other mess of it all.
I’m so against any other replacements as I have other issues, but working with alternative treatments, out of pocket money, as my hip replacement has been a horrible drama/saga.
Dear Joy,
I’m sorry to learn that you are so disappointed with your hip replacement. I think it is important to define and isolate why you’re doing so poorly. Other conditions, to which you alluded, such as having a back condition and an arthritic knee and foot, all can masquerade what the real or most debilitating problem is. These other conditions need to be defined and hopefully ruled out as the primary source of pain.
I find it curious that you report having a good result for the first five months after your surgery as this suggests that the surgery was done for the right indication, i.e., you did well and were pleased for the first five months after THR. This suggests that something changed after five months. For example, the stability of the components could have been achieved initially, but then proved inadequate so you developed either a loose cup and/or a loose stem. I also think infection must be investigated and ruled out. The first step to rule out infection is to have two simple blood studies done, an ESR and CRP. If these values are elevated, further investigation with hip aspiration should be considered.
Unfortunately, injury to the lateral femoral cutaneous nerve is a common complication after the anterior approach for hip replacement. This most often leaves the patient with an area of decreased or uncomfortable sensation or numbness over the anterolateral thigh (top, outside area of the thigh), not the entire thigh. Also, if this nerve injury occurred, I would expect these symptoms to be present immediately surgery, not five months post-op. If they did develop five months post-op, then you have to consider that it could be a manifestation of back pathology compromising a nerve root. Femoral nerve function also should be assessed.
I’m not sure why you developed a problem with your IT band. The anterior approach typically does not violate this structure. Possibly, it’s secondary to an altered gait pattern or hip mechanics.
My recommendation is to go back to your surgeon and share your concerns and issues to see if a fresh and thorough reevaluation won’t help define the problem(s) and solutions.
Good luck,
WAL
On July 17th, I had a left THR. The doctor used the posterior procedure. I’m now 6 weeks out and doing good. Not wanting to go through all the restrictions, I was considering anterior for my right hip, which would require not having it done locally since doctors here have been doing it for only 1 year. After reading your articles, I have decided not to have anterior. My doctor does not do mini posterior, therefor I have a 6″ incision. Not putting you on the spot, but would it be advantageous for me to drive 200 miles to have a consultation done by you?
Hello Larry,
If your surgeon did a great job, that is something to respect. The actual length of the incision really is not important, but rather how well the components were implanted and the hip mechanics restored. It sounds like he did fabulous job. That being said, you should have the additional surgery where you feel you will have the best chance of doing well.
The size of the incision is determined by how large and tight the hip/thigh is and how much tissue (fat and muscle) exists between the bones of the hip and the overlying skin. Sometimes, when a surgeon is working too hard to reconstruct through a very small incision, the ends of the incision tear and the tissues are traumatized. This often leads to a less than optimal component position. Remember, what you’re hoping to do is have a hip construct that will last 20 years or more. My strategy is to make as small an incision as possible, but one that allows for excellent exposure and reconstruction without brutalizing the tissues.
Best,
Dr. William A. Leone
Do either of your techniques require the traditional anterior or posterior precautions? The information I have gathered seems to indicate the anterior approach is more inherently stable, making precautions unnecessary. The posterior approach, then, is less inherently stable but may or may not require precautions. What determines the differences?
Dear Jeff,
Most doctors have and continue to implant hips through the posterior approach. Historically, higher dislocation rates were reported with the posterior approach, but it still was used for its many other advantages. Currently, the incidence of dislocation after the posterior approach has been greatly reduced due to technique and other refinements.
Because of the marked improvement in modern plastics, there is greater longevity and durability of acetabular plastic liners and larger femoral heads are used routinely which results in an improved the head/neck ratio and therefore the jumping distance for a hip to dislocate. Enhanced soft tissue techniques also have been developed which more securely close the tissue around the newly placed prosthesis and set the stage for healing.
The development of a complete and secure surrounding scar tissue wall or pseudo capsule is critical for stability. Optimal component positioning also is critically important for the best stability and longevity. Further, the extent of dissection is more minimally invasive, which also improves stability.
Because of the concerns of posterior dislocation, in the past patients were taught certain positions to avoid. Over the years, these precautions and the length of time to adhere to these limits have been challenged both by clinicians and patients. Depending on the stability and range of motion observed at time of surgery, some doctors don’t advise their patients to avoid any positions. Others continue to follow traditional guidelines.
I, personally, have not had a patient dislocate following a primary total hip replacement in many years. My advice is to consult with your surgeon regarding how stable the replaced hip is and the most appropriate rehab to follow post-operatively.
Dr. William A. Leone
My acyive 60 year old husband is scheduled to have Mini posterior total hip replacement in 6 weeks. Our second opinion doctor performs traditional and Birmingham hip replacement. Because my husband has circulation problems in his leg and vein removed for open heart surgery last year…his surgeon recommended the Mini posterior surgery. After reading your blog I’m thankful he suggested this approach. Have you ever performed the Mini on a patient 1 year after major open heart surgery? My husband has a plastic valve (done in ’86) and synthetic assending aorta and triple bypass (done in 2013)…very successful surgery. We have to get ok from cardiologist and get ekg, chest xray, etc. Just need reassurance…I am stressing he is fine. Thanks
Dear LL,
I have cared for many patients over the years with significant heart and peripheral vascular disease. It is important that these medical and cardiac conditions be optimized by your PCP and cardiologist preoperatively. Surgery carries increased risks because of these conditions, but by defining the risks and optimizing any underlying conditions, the risks can be minimized and hopefully managed. Similarly, an engaged medical team needs to be available to help with care after surgery. Although, personally I would feel strongly about reconstructing the hip through the mini posterior approach (there tends to be considerably less bleeding with this approach), other very caring and competent surgeons might feel just as strongly about using a different approach. I would recommend having an honest discussion with the surgeons you are considering.
Ultimately, you and your husband need to choose the surgeon who you both feel will provide the possible best care, based on reputation and your personal comfort level. I also recommend that you look at the track record and reputation of the hospital where the surgery will be performed, especially considering the underlying cardiac and vascular issues.
All the best,
Dr. William Leone
Question from Kevin Lee:
Does the “mini” posterior hip replacement conserve more femur and allow for future surgeries if needed ? I read about this type of mini hip replacement being done in the UK and just wondering if mini hip replacement means the same thing in the US .
Answer from Dr Leone:
Dear Kevin,
“Mini posterior” refers to the approach or tissue interval the surgeon uses to implant the Total Hip. A mini posterior approach is a modification of the classical posterior approach. It exploits the same soft intervals but it typically accomplishes prosthetic implantation and soft tissue balancing through a smaller incision and, more importantly, with less underlying soft tissue dissection.
If a mini posterior approach is used and the resultant total hip has optimally positioned components and balanced soft tissues, and was implanted through a smaller incision with less underlying soft tissue dissection and trauma, then I believe it is a benefit. Potentially there also is less pain and a quicker recovery. If the tissues are traumatized and / or the final components are not optimally positioned, then it certainly is not an advantage.
When the stem is placed in the femur, it still destroys the same amount of bone for implantation, regardless of which approach is used. If a revision were necessary, even more bone must be destroyed to remove it. Many modern-day femoral stems are considerably smaller or “more bone sparing” than well-functioning stems of the past. Some in the early period have good track records, others do not.
Sincerely,
William A. Leone
It’s been a couple months and I thought I’d drop in with an update…..over 4 yrs post op and I deal with Femoral nerve damage from Anterior, and found others who deal with the same….it may lessen with more years but who knows….Somewhere I read 15% or so end up with this..I talked 2 other people in my city, same surgeon and they have had this issue to.
Now the IT band, why who knows….
I deal with OA lower back “mess” so know I see most likely how all this has played into the surgery.
My knee and foot and ankle are messed up too since leg ended up at least 3/4″ shorter….I wear a shoe lift, but probably needed it sooner than I realized the shorter issue…
My knee is pretty stiff and pain when I walk too much, but I deal with it, it bends good, I sleep good, no pain when I do nothing, so I’m working all to do NO knee surgery…
This hip was ENOUGH to last a lifetime….. I’m 76 and use a lot of supplements to save knee and OA in general…..I am looking at other protocols for the knee too….not insurance covered, what else is new….if it’s good, it’s out of pocket…. J
Dear Dr. Leone,
Thanks so much for this information! I am an obese female and will be 62 in February. I have dealt with my hip pain and limping for over a year, can no longer perform my daily activities, and cannot sleep well anymore. I exhausted all other non-surgical options, such as physical therapy and meds but to no avail, so now plan to have a THR in March. My surgeon uses the posterior approach. After reading a few articles on anterior vs posterior including yours, I know now that his decision to use the posterior approach is the best one for me!
I have had problems with my hip for the last several yrs. It was discovered that I had a torn Labrum. They thought surgery to repair it would give me about 5 yrs. It turned out to be more torn than they thought and they had to cut about a forth of it out. The pain in my hip is strange in that I can hike uphill and down hill, bike and X-country ski but have a very hard time walking on the flat, especially after sitting for awhile or getting out of bed. Sometimes the pain goes away as I walk and sometimes it doesn’t. I never seem to know when I am going to get hit with pain. I am scheduled to have total hip replacement surgery in 2 weeks. My question is, I am a very active 67 yr old. I ski, hike (steep terrain) with a pack -about 25 pds, kayak, horse back ride, swim, water ski and bike, which is getting increasingly more difficult. Will I still be able to do all of these things? If not, what will my restrictions be? My doctor does the Posterior approach, he didn’t say anything about the mini part.
Dear Mary,
It does sound as if proceeding with a THR is appropriate, since your attempt to repair the joint arthroscopically did not pan out. Many times, the depth of the destruction that is found during surgery is much more advanced than initially anticipated, particularly as we age.
Your symptoms still sound mechanical, positional and episodic. I would not anticipate them improving with time, but rather worsening, and I can’t imagine you being able to resume the activities you described without having surgery to treat this.
Since a significant amount labrum has been removed, I think another attempt at arthroscopy would prove very disappointing and I would not recommend it.
I suspect there is significant underlying osteoarthritis related to your labral pathology. Often, as the labrum is torn, it leads to a lifting off of hyaline articular cartilage where these two tissues meet, called delamination. Once again, I think your decision to proceed with THR is the most reasonable.
I also think it’s reasonable to look forward to returning to all of the listed activities that you enjoy. Specific protocols, therapy and what positions you will be asked to avoid after surgery and for how long will be directed by your surgeon. Your surgeon will know better than anyone else just how stable your new hip is immediately after your surgery and how securely the surrounding tissues were repaired after the reconstruction.
Just because hardware in your foot needed to be removed after repairing what sounds like a calcaneal (heel) fracture, absolutely does not mean that your body rejected the metal / hardware or that your body will reject the prosthesis your surgeon will implant to reconstruct your hip.
My advice is to have a frank discussion with your surgeon and share these concerns. It’s been my experience that patients who go into surgery well informed have a better experience and seem to rehabilitate more quickly.
I wish you the best of luck,
William Leone.
In May of 2015, I had a Labial tear repaired. They thought it would give me about 5 yrs. but it was more torn than they thought and they had to cut out about 1/4 of it. I am still a very active 67 yr old, I like to ski, bike, hike (steep terrain) with about 25 pds. I ride horses, water ski and kayak. The pain I get is in the groin and a sharp pain in the buttocks, that feels like muscle pain. The pain is really inconsistent, one min I will be walking fine and the next it catches and is very painful, then it may go away or may not. I seem to be able to hike just fine up hill and down but not always on the flat. Sitting seems to irritate it the most. The doctor has scheduled me for total hip replacement in two weeks and he uses the Posterior approach, he didn’t say anything about the mini part. I am temped to wait but it is getting worse. My question is, what will my restrictions be? Will I still be able to do the things I like to do? Also, after an accident, I had 12 screw and an L shaped plate in my heel. After awhile the screws started shifting and poking up under the skin and they removed them. Does this mean my body may reject the metal of the post or cup? Thank you so much for your answer, I appreciate your taking the time to care about others.
Dear Dr. Leone,
I am a 49-year-old female. I am about to have a hip replacement and would like to know what kind of limitations I’ll have afterward. I’m hoping to play tennis, go dancing and horseback riding once I’ve healed. I already have an artificial knee that is doing great. Are these expectations realistic?
Pam
Dear Pam,
I should think that all your expectations are appropriate for the activities you look forward to, especially considering you’ve already done so well after your knee replacement. I advise both my total hip and my total knee patients to avoid repetitive impact activities like distance running. I think tennis, dancing and horseback riding are fine. In general, I would encourage you to consider all of your prosthetic joints a remarkable modern day miracle that must be cared for and respected. If your “little voice” is questioning if you are overdoing it or hurting yourself, then listen to it and ease up.
I wish you well.
Dr. William Leone
Hi guys im 43 and live in Australia and due to have hip replacement in 7 weeks but im so confused as my surgeon is doing the posterior and im off work for 6 weeks where i here people having the anterior and going back sooner and no restrictions on hospital discharge any advice
Hello Jason,
In my experience the approach used to replace a hip does not effect how quickly a patient recovers. How the soft tissues are handled and respected, the patient’s expectations before the surgery and the surgeons experience do. In my practice, patients who undergo a THR using a mini posterior or posterior approach:
1. Are expected to be out of bed (hips and knees patients) the afternoon of their surgery and at least taking a few steps if not walking.
2. Typically, most are eager to go home the very next day; many have already progressed to a cane, which they will not use very long.
3. I emphasize continuing exercises at home especially walking. Most THR patients do not need significant supervised physical therapy after surgery; they simply do well when their surgery is done well.
4. If possible and a pool available, I encourage my patients to walk and exercise in a pool and / or swim, starting at two weeks when their suture is removed.
5. Return to the work place is an individual decision. The most important variable is how quickly the person is motivated to return to work. In general, if someone is dedicated to the job, the return is very quick. Many in business or who own their own businesses will stay home for only one week and then return to their work place because they are bored and would rather be productive and busy. Other jobs, which tend to be more structured and / or more physical, may require more time off. The vast majority of my patients return to work one to three weeks post-operatively. Six weeks or longer is the exception.
Regarding restrictions after your hip replacement, this too is an area that has changed drastically over my 25 year career. In my experience, the restrictions (or those positions we ask our patients to avoid after surgery) have become much less limiting and are off limits for a much shorter period of time. I would encourage you to discuss your expected recuperation time and specific restrictions with your surgeon.
I hope you do well.
Dr. William Leone
I am 37 and have suffered from AVN since I was 14.(I have SCD) It has now become unbearable and I am preparing for surgery. First, I am a little bit scared. The doctor is planning a traditional posterior. I dont want a long recovery time as I am very active. I have insurance with very high deductible and I am scared of the debts I might incur afterwards too ( where I am planning to do it – I might not have to pay any money). About how much does this cost? Should I go for this – or should I opt for the mini posterior. Also, how about hip restructuring instead of Total Hip Replacement. Can I make an appointment with you. I am female and I weigh 115 pounds
Dear FD,
It is 100 percent normal and expected to be “scared” before surgery. Everyone is. You should feel good that you are aware of your fears and that it hasn’t paralyzed you into not acting.
Nobody wants a long recovery. In my 25 years of practice, the variable that seems to have changed the most is how quickly people recover from this surgery when done well. It is normal to want to recover quickly and return to a very active lifestyle without pain. These are all realistic goals. I would encourage you to discuss your concerns with you surgeon. I find that patients who are well informed and know what to expect prior to surgery get well even faster.
I also would encourage you to choose your surgeon first – not the procedure, approach or prosthesis. Further, I would contact your insurance carrier and the hospital so you will not be surprised with any unexpected costs. If possible, try to get in writing any verbal promises made. This too will lower your anxiety and improve your experience.
I think researching the hospital where you will have your surgery is very important. If possible, choose a hospital that specializes in joint replacement and can back that up with excellent statistics and reputation.
I wish you only the best.
Dr. William Leone
Thank you very much for taking time to reply me. I had the surgery on June 22 and I am about 5 weeks post op. I had the mini posterior approach done and it gets better everyday. Pain is almost gone and I am beginning to get back to my life. I still have a very big limp and still undergoing physical therapy. Thank you for all you do and for providing me with the information when I needed it.
I just want to thank you for the information on this site. I am Australian so no business from me but it has helped me become happier with my prospective surgeon’s judgement that he will offer me a posterior THR (hopefully the minimally invasive) when my insurance allows the procedure to occur.
Is a prerequisite for THR to have a MRI or Pet Scan? Or are x-rays definitive for determining the exact reason for THR? How does it affect the actual success of the
THR if a MRI or Pet Scan isn’t done? Thru X-rays I’ve been told both hips are bone on bone!
Does anyone ever attempt to do both at the same time if THR is determined?
What are your thoughts with regard to Stem cell therapy in lieu of THR?
Dear Kent,
If your X-rays reveal that you already have “bone on bone” due to osteoarthritis, then you typically don’t need either an MRI or Pet Scan, unless another diagnosis is suspected. Getting those studies will not change the reality that you will need THRs. Historically in my practice I performed many Bilateral THR and TKR and have backed away from that practice. I think there may be increased associated complications. I prefer reconstructing the most symptomatic side first. I then stage the second surgery as early as 2 ½ or 3 weeks post-operatively. I would rather my patient get half as much anesthesia. Most receive a simple spinal with sedation. With a bilateral procedure during a single anesthetic, the blood loss would be double and there would be a much higher likelihood that my patient would need transfusion post-operatively.
I very rarely transfuse any patients now. One of the biggest changes that I’ve seen in my practice over the past 25 years is how quickly patients get well and go home. Being discharged to a rehab unit is now the exception. Most patients after a bilateral procedure would not go home but rather a rehab unit. Most of my patients now go home the day after their surgery or the next.
I think stem cell injections will have little chance of doing any good if indeed your hip condition has already progressed to “bone on bone.”
I wish you the best of luck with your care.
Sincerely,
Dr. William Leone
I’m a 50 year old female whose been dealing with hip, leg and back pain for many years, recently diagnosed with OA, and finding that I need a right THR. I have the hospital but am deciding on the surgeon and which approach is best. I saw a surgeon who does the posterior approach only and will see another on 4/14/15 who does both approaches. The surgeon I saw said that my body structure and gait does not affect which approach would be ideal for my body. My right leg is already a bit longer than the left. I weigh 185 and am 5’4″ and realize it’s ideal to lose weight prior to surgery (working on it as always). My main concern is that I have a tilted sacrum and a very sway back. My gait is off partially due to my hip but also I believe because of my body structure. I’ve done PT and plan to continue working on strengthening my core and flexibility of those large muscles. I also regularly receive Rolfing treatments which has helped me manage pain and maintain what mobility I have. So my question is in relation to my body structure. Does it really not matter which approach I have, posterior or anterior? I have a tilted sacrum, sway back and a very large posterior.
Thank you, Lisa
Dear Lisa,
What is most important is that you find a surgeon who understands the particular complexities with your problem and whom you trust. I would then let that person decide with what approach they think they can best accomplish the surgery and deliver the best result. Choose your surgeon and not the approach or prosthesis.
That said, in general people who are longer, more flexible and thin are more easily constructed anteriorly than individuals who are very stiff, contracted, thick, and have acetubular protrusion (a condition when the femoral head wears away the central cartilage and bone of the acetabulum). Also, patients with shorter femur necks and genu varus (lower angle between the shaft of the femur and the femoral neck) are more difficult anteriorly. Either and all body types lend themselves to the posterior approach because it is more extensile (can make it bigger and release more soft tissue structure if needed).
Losing weight and strengthening your muscles pre-operatively will make surgery easier and greatly facilitate your rehab.
I wish you the best,
Dr. William Leone
When asking a prospective surgeon about the anterior vs posterior approach he told me that it is necessary to use a smaller prosthesis which would not be as stable with the anterior approach and did not recommend it for this reason. After reading your article I see there are many reasons to go with the posterior approach but nothing about having to use a smaller prosthesis with the anterior approach. Please comment.
Also if the mini posterior approach is so effective when would it not be preferred over the regular posterior approach? What reasons would there be to use the regular over the mini? Thank you
Dear Tracey,
Because the femur is more difficult to expose during the anterior approach vs. the posterior approach, many surgeons will select a shorter femoral component to facilitate reconstruction and lessen chance of fracture. Many manufacturers are responding to the surgeons’ desire for shorter stems and many are now available on the market. Many of these stems have very little if any long term follow-up, although some appear to be doing well in the short term. When we quote probability of longevity after hip replacement based on following people who had the operation, it is based on standard length stems. Time will tell if this generation of shorter press-fit stems fares as well.
There does appear to be an increased incidence of stem instability when implanted through the anterior approach, but I believe this is largely a function of the surgeon experience. Also, in the U.S., nearly all stems which are being implanted through the anterior approach are press-fit rather than cemented. In my practice, I cement an Exeter stem in a significant percentage of my patients who undergo THR . I do not want the approach to dictate the optimal construct which I hope will last 20 years and more.
A miniposterior approach uses the same intervals as the standard posterior approach but simply less tissue is released for the exposure. Every patient needs to have as limited an approach and dissection as possible that does not compromise the final implant position or create excessive trauma to the soft tissues. Operating through too small an incision and not releasing tissue that would improve exposure and result in a more balanced joint in my opinion does a disservice. It is much better to precisely release and cut rather than tear or fracture. The art of surgery should mimic a well rehearsed ballet or symphony. If it’s a struggle, then the situation needs to be reassessed. Patients who are significantly overweight (I specifically assess the amount of tissue between the skin overlying the lateral hip and the greater trochanter), who have significant long-standing contractures and restricted ROM, congenital dislocation, and marked acetabular protrusion (when the femoral head wears centrally into the acetabulum) typically require a larger incision and more soft tissue releases. This does not necessarily mean they will have more pain or take longer to get well.
I wish you a full and speedy recovery.
Sincerely,
Dr. William Leone
Everything does point to posterior being the better of the two, but first i was’nt given a choice, and much easier said to shop for surgeon, than to do it, when only one in this area takes my insurance. So im going back to the surgeon that did my left hip and left me in agonizing pain for 2 months after procedure. I actually was supposed to get both done at roughly same time but its been 3yrs with this bad right hip, mainly i was in great fear of going through that pain again, but now i think that pain will be better than this everyday pain!!
Dear Don,
I’m sorry to hear that you struggled after your first, anterior-approach THR. Having a THR is a major undertaking and it is reasonable to expect the hip construct to function optimally for twenty and more years. I would encourage you to discuss with your surgeon the difficulties and pain you experienced after the first surgery, and together explore if another plan can be created for a better outcome the second time around. That being said, in order to meet your goals, if need to leave your area and consult with surgeons in other areas, I think that is reasonable also.
I wish you the best,
Dr. William Leone
Hi,
I had an anterior approach hip replacement. I’m a very healthy long distance bicycle rider. I’m 56 years of age, 6′ 1” and 180 pounds. Last summer I wiped out on my bike and snapped off the top of my right femur, with a diagonal break. I have/had arthritis in my hips. I went with a total hip replacement. I’m getting close to needing my left hip done. I can still do 30-45 mile rides, but I need to take something before each ride, because of the undone left hip. About my surgery: I had to wait 30 hours before surgery, two days later I was released, within two more days I stopped using my walker. In another day I was able to take short walks without any limping, etc.. I was released to go back to work after only 10 days. I needed no physical therapy at all. I was told to wait 6 weeks before I resumed my exercise regiment. My first bike ride was 22 miles without any problems. It’s been 8 months now. The only problem I’ve had post hip replacement is some on/off again groin pain. I had to cut some strength exercises out— leg lifts, hip sled. The leg lifts really aggravate the front of the hip. I’m considering this mini posterior approach. Should I be though? It would be interesting to hear what you have to say… Doug
Dear Doug,
Overall, it sounds as if you’ve had an excellent result and wonderful recovery following your hip replacement. My clinical impression is that more patients experience some degree of residual groin discomfort or tightness after the anterior approach as compared to the posterior approach, but that it tends to resolve with time. To have your other hip replaced through a different approach is a decision you need to make with your surgeon. If you feel confident in your surgeon, I would discuss it frankly follow his or her guidance as to which approach and prosthesis are most appropriate to give you the best result.
I wish you the best.
Dr. William Leone
Dear Doctor,
In 2013 I had a THA done on the left hip. Back then my surgeon advised me to perform a posterior surgery as opposed to anterior saying that I was overweight, short and a very muscular person and it would be easier and safer to do so. Considering I had no idea about differences between the two approaches, I said OK and surgery did go well and I was back on my feet in no time.
In 2014 I had to do another THA, this time on my right side. When discussing the options, my surgeon all of a sudden suggested performing anterior approach. She provided all kinds of “benefits” with this approach, as faster recovery, less motion restrictions et.al. For risks she mentioned all the usual I knew about from the first surgery – blood clots/loss, dislocation, etc. She never though mentioned an increased risk of damaging femoral cutaneous nerve or possible muscle damage that would turn into improperly heeled muscle as a result.
After reading your article on disadvantages of anterior approach and also doing extensive online search about this subject, I came to realize that anterior approach was definitely a wrong choice considering my physical build – short, muscular, overweight. Results of the surgery – numbness in the right thigh, inability to stand on the right leg, muscle atrophy – all confirmed by EMG and second orthopedic surgeon. My two questions are:
1. Are my findings that posterior approach in my situation would have been more appropriate?
2. What, if anything, can be done to revive femoral nerve and get my thigh muscles back in normal?
It’s been six months since surgery, my operating doctor keeps feeding me with “let’s wait another month” stuff. But I feel that time could be lost and all my symptoms may become irreversible.
In hopes that THA would let me live my normal life without arthritis, instead I can barely walk more than 100 yards without having to stop, my gait is crooked causing lower back problems and my personal life is less than perfect.
Sincerely,
Stan
Dear Dr. Leone,
After a slip and fall at work 2 1/2 years ago I need a THR on my left hip. I have been in excruiting pain and unable to do everyday normal activities. I have been doing ALOT of research about the different approaches to THR and looking for the absolute best surgeon. One thing I do not want is any muscles or tendons cut in the procedure. Your article is the first I’ve read in which no muscle or tendons are cut in any approach other than the direct anterior approach. A couple of things I am hoping you will explain using laymans termology. What do you mean by painful anterior scarring and soft tissue exposure and trauma? Also I have read that there is a sharp learning curve that must take place in order to do the direct anterior approach. Why is that? Lastly, where can I find a great surgeon that takes FL Workmans Comp? Thank you, Lisa Blumthal
Dear Lisa,
Your primary goal should be to find a surgeon in whom you trust and who will take the workman’s compensation insurance. Once you find that doctor, then you need to put your trust in him or her to help you solve this horrible problem so you can return to being active and productive.
The anterior approach exploits an interval between muscles that cross the front of your hip and thigh. This interval must be developed and the muscles must be separated in order to reconstruct the hip. In some individuals, it takes much more force and dissection in order to accomplish this (typically, there is significantly more bleeding from an anterior approach compared to a mini-posterior approach). Some people also tend to form scar tissue and contracture more readily than others. Also, some body structures or anatomy makes approaching a hip anteriorly much more difficult than others. Because the dissection is over the front of the hip, a number of patients will experience residual pain and tightness anteriorly (in the front of the hip) at least early on.
Surgeons do not cut across muscles. “No Muscles Cut” is for billboards. Intervals between muscles are separated or muscles are separated in line with their fibers without injuring the muscles’ innervation. The most important thing is that tissue is handled gently and trauma is minimized, whichever approach is used. Don’t let PR marketing confuse the big picture.
I again suggest you concentrate on finding a surgeon in whom you have faith and then trust that doctor.
The best of luck,
Dr. William Leone
Dear Stan,
The femoral nerve functions to extend the knee and also is responsible for sensations over the anterior and medial aspects of the thigh, medial shin, and arch of the foot. The hope is that your nerve injury will recover with time. The rule of thumb is that recovery occurs over a 12-18 month period following injury. The earlier the recovery begins, the better chance for a more-complete recovery. Also, be aware that as the nerve recovers, the smallest C fibers within the nerve recover first, which can cause a burning discomfort. This is actually a good sign. Depending on the degree of injury, you may need a knee brace to lock you knee in extension when walking until the quad function returns.
Therapy is often appropriate for stretching, strengthening and electrical stimulation which helps maintain the motor end plates, structures on the muscles that the nerve branches must re-innervate. Pain modifying drugs as well and as a course of NSAIDs might also be appropriate. In my experience, people recover from femoral nerve injures more frequently and completely than from sciatic nerve injuries.
Therapy hopefully will help any contractures and scaring within your muscles that might have developed after surgery. I would stay away from narcotics. They are addictive, can cause depression, their analgesic effects are short lived and if the condition persists, you will require an increasingly higher dose to relieve the pain. What you can do is keep as good an attitude as possible and keep rehabilitating your leg. I also would encourage pool walking or swimming. It will help desensitize and help get your muscles working in synchrony.
I wish you the very best,
Dr. William Leone
Going in for THR in July. Posterior approach. Doc says once recovered I should avoid flexion with adduction and internal rotation. I am very athletic and active even with many years of pain from bone on bone arthritis so I am worried about restrictions since I’ll probably forget or something. Can’t afford a dislocation or other complications cause I’m sole caregiver for severely handicapped son. THOUGHTS?
Dear Lynn,
Fortunately, the incidence of hips dislocating after THR is very small, especially after first-time hip replacement. Irrespective of the approach that is used to implant the prosthesis, the tissues that surround the new prosthetic hip must heal and mature if the hip is to achieve stability. This complete wall of tissue that surrounds the new hip imparts stability. The healing and maturation of this tissue takes time.
Today, everything from tools to techniques has improved. We now have less-invasive techniques, better surgical methods of closing soft the tissue and more experience. Also available today are larger modular heads, made possible because our plastics are so much better than years prior. What all this means for patients is a more optimum outcome and faster healing, which can reduce time interval to return to normal activities. I ask my patients to restrict certain positions that exceed the mechanical limits of the artificial hip for the first six weeks. Most of the restrictions are removed at that time, although I still advise “common sense,” particularly for the first three or four months. Each surgeon approaches these issues individually. The particular surgeon who did your hip is also uniquely qualified to advise you with regard to the postoperative stability of your particular hip, because he or she physically tested your hip intra-operatively. In my experience, after four to six months most patients simply return to normal activity.
I wish you the best.
Dr. William Leone
I have congenital hip dysplasia which has gradually caused more pain as I’ve gotten older. I am 56 now and find that physical therapy and chiropractic care don’t seem to be helping anymore. Is THR something that can help? My problem isn’t from a worn-down joint with no cartilage. It’s from a malformation. I worry that replacing it with a differently configured socket could make things worse rather than helping.
Hello Christine,
The most common reason or diagnosis that leads me to replace the hips of young women is hip dysplasia. Often in this group of patients, their X-rays show only minimal cartilage space compromise (it may appear thinned and irregular) and I observe at time of surgery that the labrum appears hypertrophied (to compensate for lack of head coverage) and often torn. The hip replacement needs to correct the abnormal hip mechanics that lead to the arthritis. The new prosthetic socket must be medialized (placed further toward the midline) and sometimes through the medial wall of the native socket. This effectively moves the hip joint center, toward the bladder or midline, and improves hip mechanics. It also helps to stabilize the acetabular shell and prevent soft tissue irritation on the out edge of the cup. In severe cases, I will use my patient’s own femoral head, which is removed as a bone graft to help stabilize the new cup and “garden” new bone for the future. These are some of the most grateful patients in my practice.
I wish you the best of luck.
Dr. William Leone
Comments about life-long hip restrictions between Posterior, Anteriorlateral and Anterior approaches? I’m hearing ‘no restrictions’ (once recovery is done) for Anterior, but always some for the other two. I’ve never foulnd information from any doctor or research-site but that there is always no legs-crossing, no more than 90-degrees (for the most part), and no twisting for anything but full Anterior. Is AL better than P for this? And does A really have ‘none’.
Lastly, if one has had P or AL is there anything that can be done to offset the need for restricitons? I’m an avid skier and just found out I did not have full Anterior but rather AL. (tho’ I am sure I asked about it ahead of time)
Dear Janet,
I believe you are having trouble finding definitive answers and recommendations because every surgeon has his or her own recipe and experience and also the medical recommendations keep changing. Mine certainly have. Understand that every total hip, no matter which approach is used to implant it, has the potential to dislocate. Fortunately, if the components are stable (bone-in grown or cemented) and optimally positioned, and the surrounding tissues has fully healed and matured, then that risk is very small. Most individuals who have had total hip replacement surgery fall into this category and simply “resume their lives.”
The incidence of dislocations has further decreased over the past decade with our ability to implant larger size femoral heads. We can do this because of improved plastics. Hard-on-hard bearings, such as ceramic-on-ceramic as well as metal–on-metal articulations, also resulted in larger femoral heads being implanted. Very few metal-on-metal bearings are being placed today due to the serious potential of metallosis. Also, only a small percent of C-on-C bearings are being implanted at this time. Regardless, the overall incidence of dislocation for every approach is smaller due to use of larger femoral heads and enhanced closure techniques.
Every prosthetic joint has a mechanical range of motion. Once it exceeds this ROM, impingement occurs. The impingement can be between the metal neck of the stem and edge of the cup or between soft tissues. The impingement can lead to a levering out of the ball from the socket. The bigger the ball, the bigger the ROM without impingement and the bigger the “jumping distance” that would be required for the hip to dislocate. Once the surrounding tissues fully heal, they then act as a mechanical block to the ball to keep it from being able to “jump out.”
My advice would be to avoid the extremes of any motion that exceed your hip’s ROM. Even if the hip doesn’t dislocate, prosthetic or soft tissue impingement is not beneficial. I also would find out your surgeon’s recommendation regarding activities and restrictions.
What I’ve seen in my practice is that the more total hips I do, the less restrictions I place on my patients and the more active my patients are.
Good luck.
Dr. William Leone
Hi,
I was thinking of a Hip Resurfacing for my left hip and was convinced by my other top hip surgeons to stay away from it. I am a competitive tennis player in my age division. I play in the 50’s age group. I am suffering from a severe range of motion where I can’t put my left sock on or tie my left shoe, I can barely get in and out of low cars and sitting up at a table hurts too! I am deciding that my quality of life is in the toilet and need to get the THR done. What is the best stem and ball/socket combo to use for someone that ones to play tennis?
Thanks,
Brian Tinsley
Hello Brian,
The most important decision you must make is choosing your surgeon. I then would trust your doctor to select the prosthetic that would deliver the best result according to your goals and allow you to return to activities that you enjoy. That being said, I agree completely with your surgeon’s advice to have a total hip replacement and not a hip resurfacing. There aren’t any activities that you can do with a resurfaced hip that you can’t do with a total hip. I would avoid the metal-on-metal articulation. We now have too many other proven bearing surfaces available. I don’t think there is “one best prosthetic.” Some have features that are more suited to one person’s anatomy and needs than others. Again, trust your doctor. The highly crossed linked polyethylene liners are now the gold standard in this country. Many also mate this with a ceramic femoral head. A ceramic-on-ceramic bearing is also a very good bearing.
I have linked back to several blog posts below that will give you more in-depth information.
http://holycrossleonecenter.com/blog/hip-resurfacing-or-total-hip-replacement-a-candid-discussion/
http://holycrossleonecenter.com/blog/metal-on-metal-hip-replacements/
I wish you the very best recovery.
Dr. William Leone
Anterior vs. Posterior, Posterior vs Mini-posterior. Need to choose, then select doctor based on that decision. Also, is it immoral for an 80 year old to have THR and cost the nation’s health care system $25 – $35k? I understand they have good results in Thailand or India for half that. Maybe someday our nation’s health care system will measure up to that of France, Norway, Switzerland and others, in which their governments are investing half of the GDP that we are wasting. What are the experiences of other countries with THR?
Dear Cecil,
The most important decision you will make is choosing your surgeon. I then would strongly suggest you trust that person to decide what approach and what prosthesis predictably will deliver the best results.
I think the money you spend to have a hip replacement is more than just moral or justified, it is smart “business.” After all, no matter the age, it will determine the likelihood of maintaining your mobility and independence. When people loose independence and mobility, not only does the quality of life suffer, they are much more likely to develop a myriad of medical problems requiring even more-expensive and/or long-term care, including loss of independent living.
If you decide to have your hip replaced in another country, I would consider carefully who would care for you if you develop a complication such as an infection, or a major medical problem like a pulmonary emboli or heart attack after surgery. Personally, I would not gamble with my health. I also would learn about the track record of the surgeon and hospital where you will decide to have the surgery and what implant will be used. There are many different quality implants (just like surgeons and hospitals).
The best of luck to you,
Dr. William Leone
I just saw a patient with a femoral “neuropraxia” after a anterior approach THR. I have not seen this before because in the past, the complication from hip surgery were sciatic nerve injury from posterior approach. I was not aware that any of the local surgeons who is doing anterior approach. I spoke to the surgeon, he believes it may take up to 6 months to get better from this “neuropraxia”. I feel that at 10 weeks with profuse denervation potentials on the quad muscles, the prognosis is not good, even at 6 months. What is your experience and take on this ?
Dear Doctor,
Lateral femoral cutaneous nerve injury is the most common injury incurred during an anterior approach. The second most-common injury is to the femoral nerve. Nerve regeneration can occur up to 18 months following injury, but the chance of full recovery decreases with delay in recovery time. It’s been my experience that femoral nerves tend to recover more readily than sciatic nerves. I share your concern that with profuse denervation potentials 10 weeks post injury, that the patient may have sustained a more severe injury than a neuropraxia. Unfortunately, short of conservative and supportive measures, only time will tell.
I wish your patient well.
Dr. William Leone
Hello Dr. I really appreciate this website. I am scheduled for bilateral hip replacement at the end of August. My surgeon is doing posterior and my reason is I am self employed with limited Time off available and hope to be back to work at least walking and driving in 4 to 5 weeks is this possible? My surgeon has told me I will need PT 3 times a week for 6-12 weeks is this too long? I’ll be 60 at the time and I’m 5’4 and weight about 130 lbs in fairly good shape. I have been in pain for about a year and first though it was a back issue and it has limited my ability to stay as active as I would like. Can I expect any problems with the bilateral it was my choice. Thank you
Dear John,
My personal preference has changed from doing both hips during a single anesthetic to staged procedures two to three weeks apart. I understand and respect that many surgeons prefer doing them simultaneously.
I choose to do them in a staged fashion because it is a significantly shorter procedure (more than half time-wise) and some think this lessens the risk of infection. There is less blood loss with a single THR than a bilateral, hence less risk of needing a transfusion. Patients mobilize the day of surgery and typically go home the next day. In my experience, almost all patients who have bilateral THRs go to rehabs and not home. I would rather see my patients go home. I think they are happier and rehab more quickly. Patients who work for themselves are very motivated to return to work and often do so between procedures. The amount of PT you need after surgery will be determined by you and your surgeon. From what I’ve seen, most THR patients don’t need very much PT, although I do encourage exercising in a pool. Walking is the best exercise.
I wish you only the best.
Dr. William Leone
Dear Doctor,
I am a South African and need to make a decision on whether my mother (69) goes for an AMIS or traditional posterior. I am unsure whether the minimal invasive posterior is available in SA. Problem is that we have seen two doctors and both seem great but are on two extreme sides of the fence. It is a pity that medicine cannot be as definitive as science but relies on historic figures and the future outcome appears to be a statistical probability!
I love that you take time off to reply to these messages – it is commendable. Please do not take this as an attack, but your article seems biased on your experience (great results with min. invasive posterior vs not so good with AMIS) – whilst on the other hand, with one of your replies you state that surgeon experience should be considered with AMIS success rates and in other replies stating that both alternatives are good.
We are now in a situation where we have found two extremely good surgeons and we gel with both extremely well. Our insurance covers both. Both have valid cons against the others methods and pros on their method. My mom is obese, short and has osteoporosis. Your article lacks the pros of the AMIS and the cons of min invasive posterior.
Can you please on the various points in the post and perhaps also elaborate on the last point. With that said, I would have probably just done the posterior with you if we lived in the US based exclusively on the time you take to respond!
Regards,
Zarheer
Dear Zarheer,
I would emphasize choosing your surgeon and not the approach. I absolutely would not insist on minimally invasive surgery and a small incision, especially considering your mom is “short, obese and has osteoporosis.” What is most important is that the surgery is expertly done, that the tissues are not brutalized, and that the surgeon can see what he or she is doing. Every surgery should be done with as minimally invasive approach as possible taking into account these other critical factors. The surgeon will be building a construct that hopefully will last her life time and change her life profoundly.
I will let you in on something personal. I have never operated on another surgeon who asked me to make as small an incision as possible or use the minimally invasive approach. (Of course, I do.) Rather, they say “Bill, please just do what you have to do and do a great job.” …………..…. And, I Do.
Sincerely,
Dr. William Leone
Dear Dr. Leone,
I am a 73 year old woman who has been having severe hip pain for the last seven months. I did have a total knee replaced two years ago. Both problems are on the right side of my body. I am experiencing pai. Getting in and out of cars, and turning over in bed. My husband tells me that I cry out in pai as I turn over during the night.
My worry is that I will end up with one leg shorter than the other. I also have undiagnosed neuropathy in both legs from the knees down. I don’t know if this stems from the knee surgery but I do not believe so because I was well for about a year and a half.
I would like your opinion on the stem cell injections as I am really afraid of the second surgery on the same side of my body. I do not have dials and no one seems to know where the neuropathy stems from. I did have numerous blood tests, MRI of knee and hip, total body scan with radio active injection, X-ray knee and hip etc.
I really don’t know where to go from here. I am concerned that I may have a pinched nerve and that that is what is causing all this pai as the pain is severe only in certain positions but when I am tired I also have a throbbing pain in the sciatic region….talk about the golden years…I thank you from the bottom of my heart for the kindness and caring that you do in answering all these questions.
Mickey Lavoie
Dear Mickey,
I am so sorry to learn that you are struggling. The source of your hip pain must be diagnosed. If it is from intra-articular hip pathology such as osteoarthritis, which is very common especially in your age group, then most likely stem cell injections will not be affective and you would benefit from a total hip replacement. I take care of many individuals who have a total knee and hip replacements on the same side. The vascular supply of your leg must be assessed preoperatively as part of you work-up, but most do very well. Also many folks develop peripheral neuropathy in their lower legs, which also becomes more common with age. A neurologic evaluation is appropriate to rule out reversible causes, but most work-ups do not elicit the exact etiology and usually symptoms only can be managed at best. Achieving legs that feel equal in length after surgery is imperative. Sometimes, it simply isn’t possible to accomplish. I believe this is an important discussion you should have with your surgeon preoperatively.
Finally, many people who are struggling with hip disease experience lower back pain or even sciatic discomfort. Your back does need to be evaluated as well. Fortunately, many folks who experience back symptoms before THR report improvement or resolution after.
I wish you only the best,
Dr. William Leone
I haven’t dropped in here for a while but here I am almost 5 yrs post op Anterior and Femoral Nerve Damage is very alive…whole thigh is numb, IT band is still very sore and numb. Thigh feels so Heavy and I massage that area a lot. What I’ve been able to achieve is find two nerve supplements that have taken away the burn/tingle on my thigh. It’s Inosine and Sphingolin. OTC nerve supplements suggested by a naturopath.
I try not to bring up my “mess” but it’s hard when it’s with one 24/7. My walking is very limited, shoe is built up as leg is shorter and in recent months I’ve realized my leg is bowed. Better luck to you all.
Dear Joy,
I am so sorry to learn that you have had such a bad experience after THR. While it is a surgery that does help many, many people, clearly you are struggling. A femoral nerve injury is devastating and is more vulnerable during an anterior approach than with other approaches. Thank you for sharing with others the “nerve supplements” that you’re finding affective.
I wish you well. My hope is that some of these symptoms will improve with time.
Sincerely,
Dr. William Leone
I, too, am struggling which approach to have. I have seen 2 doctors – one doing posterior, the other anterior. Recently the doctor doing anterior decided because of thin bone, he should do direct lateral approach. Can you explain it to me as he didn’t go into detail.
Dear Sue,
I would focus on the individual doctor, not the approach that the individual choses to use, to deliver the best result. Each approach you list has advantages and disadvantages. At the end of the day, I promise, it is not the approach but rather the person who is doing the surgery. The rest is marketing. I often suggest to my patients that they speak to other patients for whom I’ve cared and to whom they can relate to learn about their experiences. In has been my experience in life that if others are happy and had a good experience then that speaks strongly to me, if I were to do the same thing.
I wish you a full and speedy recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
As for doctors, the surgeon I had came highly recommended. I spoke in person to probably 4-5 of his success patients and went with hearing from them. I’ve since met 3 others who ended up with the mess that I’m dealing with also.
I didn’t spend time on boards talking for eons about people’s outcomes….probably a good thing I didn’t…
I don’t know what happens on that table…was he in a hurry on Friday afternoon. I went in with high expectations of coming out so much better off and here I am 5 yrs out limping more than ever and a NUMB thigh and worse knee and weak ankle. Yes, I’m angry.
All:
I recently had a spontaneous hip fx and was diagnosed with hip displasia. I am a 53 year old active, distance runner. I decided to stick with my trusted orthopedic surgeon (who did two knee scopes on me) who believes the minimally invasive posterior approach is the safest approach. I was discharged within 24 hours. Back to work/driving in 10 days. I will need the other hip done within the next 6 months, and despite all the “talk” of the anterior approach- I can use myself as the best judge to the best method. Of note, I am a RN with 30 years of experience and took this decision very seriously.
Dear Sue,
Thank you for sharing. Others will be empowered when they read and relate to you and/or your experience. Personally, it I were caring for you, I would have advised you exactly as the orthopedic surgeon who took care of you did. The mini posterior approach works wonderfully and predictably when expertly performed. Clearly, yours was. I still maintain that by far the most important decision patients must make is choosing the surgeon who will do their surgery and take care of them, then trusting that individual to choose the approach, prosthesis and make a million other decisions that deliver as perfect a result as possible.
I wish you the best of health.
Sincerely,
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Thank you so much for taking the time to inform us! I’m ready to have the surgery, having been basically bone on bone for several years. I have two questions – one, how realistic would it be to try to have both hips done at the same time? My second question relates to something you mentioned earlier regarding checking the “published” track record of the surgical team – if I use an HMO, how do I find that information, and how do I know it hasn’t been skewed to give more favorable results (“lying with statistics”)?
Thanks again for this great blog!
Dear RC,
Currently, I seldom do bilateral THRs under a single anesthesia but instead stage the surgeries 2 1/2 to 4 weeks apart, depending on my particular patient and his or her needs and desires. For many years, I performed bilateral THR and bilateral TKR procedures, but have backed away for a variety of reasons. If I do a single hip or knee replacement, that patient is out of bed standing and, in most cases, walking the afternoon of surgery. This is not true for bilateral cases. Being out of bed and moving soon after surgery adds to a patient’s safety and speeds the recovery.
The surgery time is much less with a single joint and therefore the sterile surgical instruments are opened and exposed to the environment for a shorter time. Many believe that this results in less risk of infection. Also, when a single joint is replaced versus bilateral, there is significantly less bleeding and hence a much decreased need for transfusion. Finally, because my patients are walking the day of surgery, most want to go home rather than to rehab. I believe going home is very therapeutic and often safer. Almost all bilateral THR or TKR patients go to a rehabilitation facility after their acute stay, not home.
Studying a hospital and physician’s track record before you commit is important. Many patients approach this by researching “online” and speaking to other patients who have been cared for at a particular facility. I think speaking to a patient with whom you can relate and who has been treated by the physician you’re considering also is invaluable. If possible, speak with other health professionals who work at the hospital or at least in the same geographical area.
When studying the hospital credentials, try and learn how many joint replacements are performed at that hospital each year, their infection rate and their 30-day readmission rate. I think it’s reasonable to request a tour of the facility where you’re considering having the procedure. If you’re impressed by how clean it appears and the movement and professionalism of the staff, that obviously is a good sign.
Many wonderful physicians are part of various HMO panels. I believe choosing your physician is the most important decision you can make. Once you’ve decided, you then need to trust that he or she will take the best care of you possible to deliver the best results.
I wish you the best of luck.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello Dr. I am a 70 yr old female with a 4grade thickness loss at acetabulum and head of femur. Also on MRI there was a cyst (good size). I was told the joint lubricant had migrated into the hip bone creating the cyst, There is effusion in the joint and stress areas. Not sure exactly what that means. Other health issues include congenital heart ASD corrected about 12 yrs ago with an amplatzer occluder implant by the right femoral approach resulting in possible femoral nerve compression, Lateral right leg numbness and leg discomfort since the implant, Groin pain and restriction in extending the right leg back has been a problem for some time and masked the fact that at least a portion of my increasing pain was from my hip. Glad that after lots of PT and massage and medial branch block for back issues with NO!!! results, I decided to see and orthopedic doctor was advised to have THR. I am just under 5 ft and weigh 185. Also congenital pulmonary hypertension (PA pressure about 52) and have hashimotos hypothyroid, and two additional auto immune issues ( alopecia and psoriasis of feet),and hypertension. No specifics were given to me from the orthopedist . He is highly respected by the medical and chiropractic community, so i plan to have a appointment to discuss his plans for my surgery. I have been less active this past year and am concerned that losing weight prior to surgery might be an issue, Am also wondering about my auto immune issues and the implant. Thanks for giving us patients the kind of information we need to be more educated as to what questions to ask. Would appreciate any input you might have on the auto immune issue, and weight etc.
Dear Ms. Peters,
I believe a THR will benefit you tremendously. It is important that you find a doctor who is experienced in caring for people with complex issues. Finding the right surgeon is critical, because your care is about so much more than just fixing your hip. Being cared for in a hospital that specializes in joint replacement and has an extensive specialty medical staff also is key.
Prior to surgery, you need to be evaluated by your primary care doctor and any other specialist who helps manage your care, so the conditions you have can be optimized.
I wish you a full and uneventful recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Your blog on anterior vs posterior approach was very informative. I am wondering if having mild hip dysplasia is a factor in which approach is used. I tore my labrum at age 43 and only discovered then that I had bilateral dysplasia. I had my hip scoped which bought me 8 years, but need a THR now. Since my acetabulum is too shallow, and other angles are “off” as well, how does the new cup get positioned correctly? Also, since I am only 51, I am concerned about component longevity.
Dear Angela,
I will reiterate what I know to be true. Choose your surgeon. With mild dysplasia, positioning and implanting the new cup usually is not more difficult than with other conditions. Typically, the new cup will be medialized to gain coverage and correct the abnormality that lead to your arthritis.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Thank you for this great informative discussion. It is nice to see honest Q&A versus a marketing page. I am planning to have a THR this summer. I am going to get evals from 3 docs. It is a mix of anterior & posterior. Dr Leone, you make the point several times that the surgeon, not the procedure is most important. What do you consider to be the most important factors in choosing a surgeon? What are your thoughts on the use of robotics? If I can put you on the spot…. If you were in Los Angeles and needed a THR who would you choose to do your surgery? Thanks again!
Dear Phil,
Fortunately you live in a part of the world where there are many capable orthopedic surgeons. I think seeing several surgeons for different opinions is good judgment. I would suggest seeking out doctors who specialize in hip replacement surgery rather than general orthopedics. I would look for a surgeon who is busy, has a strong track record and who practices at a hospital with a stellar reputation and where many joint replacement surgeries are done. I would consider talking to other patients who had their hips replaced by that physician and learn about their experiences. If they are really happy, then you probably will be as well. Finally, I would choose a doctor with whom you connect and whose staff is engaged and knowledgeable.
I wish you a full and speedy recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone,
I would like your opinion. July 2013 my left hip was scoped for a labral repair. It healed well but then I got major psoas pain which a cortisone shot helped. This left hip remained tender based on my exercise level which I did modify but always my hip had some soreness.
Soon my right hip started bothering me. I had an MRI by a different hip doctor (a preservationist) who diagnosed me with a birth defect (hip dysplasia). I had no inkling of this till he showed me on the x-ray. The first surgeon never mentioned this condition at all. I have since read that hips with this condition might get worse after labrum repair due to this structural defect.
Doc, I’ve worked out and been physically active forever – running, biking, skating, etc. Until now. I have had to modify my activity level by cutting back greatly and also trying new activities that might not strain my hips so much(tried water walking in the deep end which cause deep pain for 2-3 days afterwards). I walk a lot in my job and bend lots (work with children) and sitting causes pain due to impingement. Driving hurts too. I sit on a cushion in the car to lift me up.
I have read your articles about procedures (anterior vs posterior). I can’t find anything that addresses replacing a hip that is dysplastic. I am now 59, still in good condition but that is being compromised by lack of working out as my hips get sore from most everything I try.
I have written to you to learn what are the surgical considerations for someone with shallow hip sockets like mine. My doc said the angle of my hips is not the worst but also not the best. I thought the newer procedure on the special table was the best way to go.
But after reading your articles, I am hesitant about that choice now.
My physical life is diminished. I try not to let it get to me, but it causing me to feel handicapped. I saw a hip surgeon last year for an opinion, but because I had almost no arthritis on the x-ray he said he saw no need for surgery. But I am now in chronic low grade pain that’s getting worse and don’t know what I should do. I plan to retire from working full time June 2017 and am concerned about having appropriate insurance after that. With much respect I look forward to your reply. Thank you.
Dear Jo Anna,
Hip dysplasia is a very common underlying cause of hip osteoarthritis. Imagine your femoral head lacking full acetabular coverage, resulting in an overloading of the superior aspect of your socket, hence the cartilage and labrum becoming damaged and ultimately breaking down. If an MRI demonstrates no cartilage damage or subchondral cystification (the development of degenerative cysts), a repairable labral tear and minimal dysplasia, then a hip arthroscopy may be considered. Recognize that the underlying etiology is not being corrected by this procedure, so relief of symptoms probably will be temporary and possibly partial.
Honestly, most 59-year-old active women do best with a well done THR. This treatment is much more definitive and predictable.
When a dysplasic hip is reconstructed to THR, it’s important the abnormal mechanics are corrected, typically by medializing (closer to the midpoint of the body or bladder) the cup. This absolutely does not require a special table. It requires surgical insight and skill to accomplish.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dr. Leone, I am coming in to see you for an appointment for a THR to my left hip. I am a!so told by the orthopedist who referred me that I need arthroscope on my right hip. Do you also do arthroscope surgery? If so, is it possible to have both hips done at the same time? Thank you. Gary
Dear Gary,
I’m pleased that you will be coming in for an appointment. I do not do hip arthroscopy. If I think you may be a candidate, I will refer you to a doctor in our area that does. I’ll know a lot more after we meet and I review your X-rays. I definitely would not recommend a hip scope and THR during one anesthetic setting. Further, rehab after hip arthroscopy often requires partial weight bearing on the operative side and that would be difficult with newly operated THR on contralateral side.
Sincerely,
Dr. William Leone
Dear Doctor Leone,
You are to be commended for taking the time to answer our questions. I wrote to you in January, now my surgery is in a couple of weeks. You helped me tremendously in my research of the track record of my HMO, now I have one more quick question to run by you.
My surgeon mentioned also cutting something to “free me up” at the same time he will be doing the posterior approach surgery. I assume it’s something near my groin. Have you heard of something like this, and if so, is it worth it? Just getting your thoughts – I will discuss it more with my surgeon at the pre-op meeting. Thanks!
Update – what he’s cutting is the “adductor” – so my question is the same – is this just a normal part of some THR’s? The surgeon was not at the pre-op meeting, but the PA assured me it was not that big of a deal (but to me, ALL surgery is a big deal!). Thanks again!
Dear RC,
Soft tissue contractures often are associated with long-standing arthritis. Sometimes during surgery it is necessary to release particularly tight structures to expose the joint for reconstruction or to better balance surrounding soft tissues after reconstruction.
Adductors refer to a group of muscles that insert into the medial (inner) upper femur and often become contracted with an arthritic hip. In my experience, usually releasing the ileopsoas tendon insertion onto to lessor trochanter and medial hip joint capsule, and then manually stretching the leg into an abducted position after THR reconstruction, obviates the need for formal release. All of these releases may be necessary as part of the surgery and patients do well.
My recommendation is for you to discuss this with your surgeon if you have further concerns.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Hello Dr Leone,
Spring 2014 had trouble playing tennis, hip kept feeling like it was popping out of joint, groin pain, aching. July played my last match when I buckled. Diagnosed possible labral tear. Had arthroscopy in Jan 15, cleaned up tear and arthritis. Now 1 yr later don’t have buckling/giving out but a lot of pain is there and after walking around, after about 20 minutes it hurts to lift leg forward, also good hip starting to hurt. Will meet with doctor soon but when I was finally able to really exercise after surgery I overdid it and developed plantar fasciitis. It’s been 9 months(I’ve had it 2x’s bf and got rid of it and have tried everything and no results this time). Talked to my foot doc and we decided on the Topaz procedure which has good results. I was thinking of doing that 1st, maybe April(I’ll be in boot 4 weeks), and then the PTHR in either Sept or next Jan when I have free time. Would you recommend treating plantar 1st? I’m 51, 5’9″ and 148 and want to get back to tennis etc, this has been long frustrating process.
Thank-you
Dear Georgia,
Usually a hip problem is addressed before a knee or foot problem because by solving the hip problem first, the knee or foot often improves if the pain is referred from the hip (more common with knee pain) or if by addressing the hip, the body mechanics and the fluidity of gait improve. That being said, if the foot is now a much bigger problem than the hip, you may have to deal with that first. I assume PTHR is referring to partial hip replacement. If you’ve had a failed hip arthroscopy, almost certainly you also have acetabular pathology and a total hip rather than a partial hip replacement may give you a more consistent, longer-lasting and more perfect result.
I wish you a full and speedy recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone,
Ten years ago I had total hip replacement on the left at hss…. posterior surgery . Long recovery but all is well. I now need the right hip replaced. Everyone I know that has had both posterior and anterior surgery say not to even consider posterior. I have seen 4 surgeons. It seems that whatever their particular approach is that is what they “sell”. I am looking at how many hips they have done and where they are doing them. I am terrified of nerve damage as I am very athletic and a previous professional ballet dancer. I am 63 years old, 5’4″, 115 pounds. I am allergic to narcotics . I understand that most surgeons now do a spinal rather than general anesthesia. Do you agree? I am totally confused and don’t know which procedure to choose. I am seriously looking at the infection rate at each facility. It is difficult to get that from information which I find curious. Why would the doctor not have that at their finger tips? Apples to apples which procedure has the lowest incident of complications? I have been told that I can fly 48 hours after surgery?? The doc I saw yesterday said 4 weeks. No one tells me the same thing? I am feeling like this is a business like everything is else. So frustrating.
Dear Michele,
Your frustration is completely understandable. Many others feel the same. The questions you’re asking are 100 percent appropriate. Fortunately, you have already experienced a THR and have done well. That means you have an excellent track record. When done well, your body does well with this technology. Choosing a surgeon based on his or her experience and complication rate also is “exactly right.”
My strong advice is to choose your surgeon, not the approach. In the right hands, both approaches do great. In a very positive way, surgical techniques for both anterior and posterior approaches have evolved wonderfully since your surgery was done 10 years ago. Select a surgeon based on your impression of that individual: how engaged was he or she in your care, will you have access to that person as well as his or her team before and after surgery? Is the hospital where the surgery will be performed also “top rated?”
I encourage my patients to talk to other patients for whom I’ve cared and learn about their experiences. I encourage you to do the same. If they’re really happy and got well quickly, you probably will too.
The vast majority of my patients have their surgeries with a simple spinal with IV sedation so they are sleeping throughout the procedure . I prefer spinal anesthesia when possible because fewer drugs are used and often the experience is gentler. What has changed the most in my career, once again in a very positive way, is how quickly patients start walking (day of surgery), and go home and return to their active lives after THR, as compared with just a few years ago.
I wish you a full and satisfactory recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Consuming excessive-fibre and wholegrain meals will assist to keep you feeling full, and will be
more nutritious, too.
Hey, thanks for the forum topic.Thanks Again. Really Great.
I have had both hips replaced about 13 months apart, one anterior and one posterior, and there is no doubt that I would recommend anterior. Not only was my recovery twice as fast with the anterior, there was very little pain in comparison.
Dear Tim,
I’m so pleased to learn that you had a good experience. It sounds as if you had a wonderful surgeon. Thank you for sharing.
It’s interesting that when we critically analyze all the variables that ultimately make up the experience that one person has compared with another, or that one person experiences on one side versus the other, we come to recognize it’s not so straightforward. Many, many interactions and decisions go into the final result as well as someone’s perception of his or her result and experience.
Even in my practice, which is starting its 27th year, we continue to refine the surgical procedure, pre- and post-operative instructions and rehab (this is huge), pre- and post-operative pain management, and even anesthesia. Simply, we keep trying to get better. Again, considering my own practice, I routinely see my patients recover faster and easier after their second hip or knee replacement because they are more confident having had a good first experience.
Surgical approach is important but it’s just one of many important variables. Once again, it sounds as if you had a wonderful surgeon, which is the most important variable.
Dr. William Leone
Dear DR Leone,
I live in Staten Island and need rt hip replacement. The surgeon I expect to use does the Direct Anterior approach. After reading your article I am concerned about the issues you discussed. The surgeon does about 200 a year and people say he has a good reputation. I am about 5 6 and 185 lbs, age 58, he did not think the weight was an issues. My legs are very muscular and trim. Should I look to another approach and surgeon? Thanks for any feedback. Ken
Dear Dr Leone,
I live in the UK so again I’m afraid I won’t be able to consult you personally! But I’m impressed with your blog and responses, so am writing to ask you about an apparently ‘new’ procedure in which the surgeon uses a customised implant, utilising pre-operative 3D CT scanning.
I am a 67 year old woman who has danced semi-professionally and has always been very active – including doing Ashtanga yoga and caopeira. However, I now have quite severe OA in my right hip – apparently I have no cartilage left and have been told by a surgeon that I am ‘just lucky’ not to be in constant pain. I am now bracing myself for THR surgery within the next year and am wondering if there is any big advantage in trying to have this done by a surgeon who offers the customised implant, as above.
Your thoughts on this will be welcome!
Jenny
Hi Jenny –
Good question. I would also like to know about the customized implant, as I haven’t yet heard much about it. I wish you luck on your journey.
Best…..Di
I am a 55 year old with a labral tear and moderate arthritis. I was initially sent to a surgeon to consider repair but he said my chances of being happy with the outcome were only 30% and suggest a THR. Initially I was hesitant of THR thinking I was way too young for something so ‘drastic’ but Ive now been miserable enough long enough that I am welcoming the idea of surgery. The surgeon I went to said he does THR using a lateral approach. He also used the term anterolateral. Can you explain this approach? Can you compare/contrast to the other approaches; posterior, mini posterior, anterior? Thanks!
Dear Tami,
The anterolateral approach or Watson Jones approach is one of the classical hip approaches that can produce excellent results when utilized for THR. It exploits the inter-muscular interval between the tensor fascia lata and the gluteus medius. Because the gluteus medius and minimus lie over the anterior capsule and insert into the greater trochanter, it does require greater trochanter osteotomy or more commonly a partial elevation of these muscles from their insertion, which can lead to damage. There is some concern that this weakens the abductor and leads to a limp. Many studies suggest that any limp or clinical weakness resolves after approximately three months.
There are many effective approaches and techniques that allow implantation of a total hip. All have advantages and disadvantages. In the hands of a master, all can produce wonderful and predictable results. My advice is to focus on finding a surgeon with whom you are comfortable and have the best chance of doing well. I think it’s always beneficial to speak to other patients who have been cared for by that physician and learn about their experiences and results.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Six months ago I had a right posterior THR due to severe scfe; now my right leg is 5/8″ longer than my left leg. Because I have scfe also in my left hip, I will have to have it fixed too. Seeing that a THR is considered major surgery, my question is, should I have my left hip done sooner than later to address the length difference or wait until I can no longer tolerate the pain? Thanks
Dear Thomas,
Most patients decide not to wait as long to have their contralateral hips or knees replaced after having undergone a successful surgery on the first side. With degenerative osteoarthritis of the hip developing secondary to a “severe” slipped capital femoral epiphysis (scfe), recreating normal hip mechanics after THR may have necessitated lengthening the first hip. Reconstructing the opposite hip hopefully will result in legs that feel more equal.
Some patients report that symptoms increase in the not-yet reconstructed hip because of the leg length inequality. More likely, it’s because one’s activity increases after the first THR. If you are minimally handicapped with discomfort from the non-operated hip and the leg length difference is tolerable or easily managed with a shoe lift or modification, I would consider waiting. If, on the other hand, the leg length difference is creating hardship and possibly discomfort in other joints such as the lower back, knee or ankle, I would consider proceeding with contralateral THR sooner rather than later.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone:
A THR is in my future. The activity that I wish to have the most success with after the surgery is ballroom dancing. I do participate in competitions and showcase presentations. So my concerns include having the range of motion to perform moves like promenade where my body is roughly facing forward and my right leg will take a step left across my body at about 90 degrees.
Does either procedure in this discussion present restrictions or advantages for this sort of movement? Also, if a surgeon knows in advance that a certain range of motion is desired, can they provide some adjustment in surgery to help accommodate that desired movement? Do you have any advice or ballroom dancer THR stories to share? Thanks
Dear Mark,
I have many patients who are accomplished and passionate ballroom dancers. I would anticipate that you would be able to return fully to your activity once the tissues around your total hip heel. I would not change the position of the components. I don’t think one surgical approach is better or worse than the other for you to accomplish this. It is critical at time of surgery that an excellent range of motion be created without impingement. What is most important is choosing your surgeon.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I am a sixty five year old active male and need THR on my right hip. Before my hip problems, I really enjoyed playing golf and would like like to play again after surgery. My surgeon wants to use the posterior approach and indicates that I eventually should be able to play golf again. I have the surgery planned, but then another medical professional warned me that the posterior approach will limit my twisting range of motion and prevent me from playing golf. He strongly recommends the anterior approach as the only way to go. I am thoroughly confused at this point. Do you have any thoughts on this issue? Any feedback will be appreciated.
Thank you,
Kenneth
Dr. Leone,
You saw me in your office yesterday (I am 48 years old) as I had complications following a THR of right hip anterior approach with revision 4 days later for a slipped acetabular and then last week I had a dislocated hip. I still have some questions I hope you can answer as this is so distressful for me. If I have a 2nd revision of my right hip is it posterior approach or the mini-posterior approach as you discuss above? Do I have a high percentage of hip dislocation after a 2nd revision done posterior way if so what is my chance of another hip dislocation even if I do the surgery again? I read hip dislocation is 28% higher after a revision, is it more then 28% after 2 revisions??? Does my prothesis not last as long since I am now doing a 3rd surgery? How long will my hip replacement last in your opinion? Do I have a risk of fractures during a posterior right hip revision due to my prior complications already? Will I be able to dance, hike, bike, swim, exercise after a 3rd surgery? If so, how long until I can get back to normal living? I feel good now and walking good now but feel so disabled as I don’t know if my hip will dislocate again….I am sorry if you may have responded to some of these questions already as it is so much information to absorb and I don’t want to make a wrong decision again. thank you for your time…
I am a very active and young 69 year old female who had a THR on my left side 5 years ago. I have done everything I can think of to preserve my right hip, but sadly this too needs replacing. I don’t know what type of procedure was used for my first op but it was sucessful and now can do a half lotus position with no problem.I do find however that the muscles at the front of that leg are not as strong as my unoperated right leg and lifting the left leg to a vertical position in yoga, when lying on my back, is quite difficult. I would rather this not happen with my right leg when I have the THR in Jan 2017. I have a good surgeon (same one as last time) but I don’t know how he would feel about my asking if a mini posterior (or posterior) procedure be carried out, so as to preserve as much strength in my right leg as I now have.Do as many muscles need to be cut in the mini posterior procedure? Thanks so much for your help, very grateful.
Dear Carolann,
Share your concerns with your surgeon. Clearly, he or she has earned your respect and confidence. It is important that the individual who ultimately implants your next THR uses the approach which he or she feels comfortable with and has the best chance to deliver the optimal result. I would not recommend pushing your surgeon to use one specific approach or another. I think it perfectly “ok” to discuss different approaches and ask for an opinion. I would discuss fully your goals and concerns. I suspect that your surgeon has continued to refine his or her technique based on experience over the past five years, in the same way I have. We are always refining and trying to make it better.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Carolann,
Share your concerns with your surgeon. Clearly, he or she has earned your respect and confidence. It is important that the individual who ultimately implants your next THR uses the approach which he or she feels comfortable with and has the best chance to deliver the optimal result. I would not recommend pushing your surgeon to use one specific approach or another. I think it perfectly “ok” to discuss different approaches and ask for an opinion. I would discuss fully your goals and concerns. I suspect that your surgeon has continued to refine his or her technique based on experience over the past five years, in the same way I have. We are always refining and trying to make it better.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
Dear Dr. Leone, I am having Makoplasty ( robotic imaging) to my right hip in February. Is it really as good as it sounds? Help.
Thank you, Rita
Dear Rita,
This robotic technique can assist in producing an excellent result. It helps the surgeon implant the acetabular component in a very precise position. It is not a substitute for excellent surgery. I suggest you discuss your concerns with your surgeon. It’s reasonable to inquire about his or her experience using the Mako robot. It’s also reasonable to ask to speak to other patients who have undergone THR using this technique to learn about their experiences and results.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible