Frequent Reader Questions about Knee Replacement Surgery
In my last Q&A blog post, I shared some of the most common reader questions about hip replacement surgery. Again, I will use a Q&A format to share some of the most-frequently asked questions and concerns about partial and total knee replacement surgery (PKR, TKR). I will link back to respective blog posts where applicable.
Thank you for your readership and my hope is that you will benefit from this knee Q&A.
Bilateral Knee Replacement
Q: I had a bilateral TKR 18 months ago after AVN (avascular necrosis) from high dose of steroids and have been back to work for 10 months. My right is perfect, no complaints, but my left has increasingly become more painful. It feels like a tendon or ligament ended up in the wrong place, upon flexion/extension I get a popping feeling that causes pain in the knee along with increasing stiffness. Could this just be normal pain or a greater issue?
A: From your description, I suspect that you might have a mechanical problem with your left knee. Considering that your right knee feels “perfect,” I would expect your left knee to feel similar if the construct and soft-tissue balancing were the same as on the right side. Your description of the symptoms worsening rather than improving with time and “feeling like something is in the wrong place” further supports my concern. Technically, it is difficult to consistently and optimally implant and balance a TKR. Small degrees of component malrotation and/or soft-tissue imbalance can lead to compromised results and pain. I suggest you return to your surgeon and share your continued concerns and complaints and look for his or her advice regarding how to solve them.
When TKR Looks Good but Feels Bad
Q: I had a left-knee TKR in December 2014, after four separate arthroscopic procedures over the prior 30 years had finally left me with consistent bone-on-bone pain. Since my surgery, I’ve had a muffled “triple clunk” that causes discomfort whenever I bring my leg forward as I try to walk normally so I end up limping. When I ride a bicycle, there is a sharp pain on the outside of the knee with every “push” stroke and my skin is very sensitive; I cannot kneel on that knee at all. In short, I seem to be no better off now than I was before the operation – which is really, really frustrating – especially when all I ever get from the surgeon is “Everything looks good – there’s nothing left to do.” I have a feeling I’m a victim of “soft tissue” complications, with something just rubbing the wrong way against the components. What does this sound like to you?
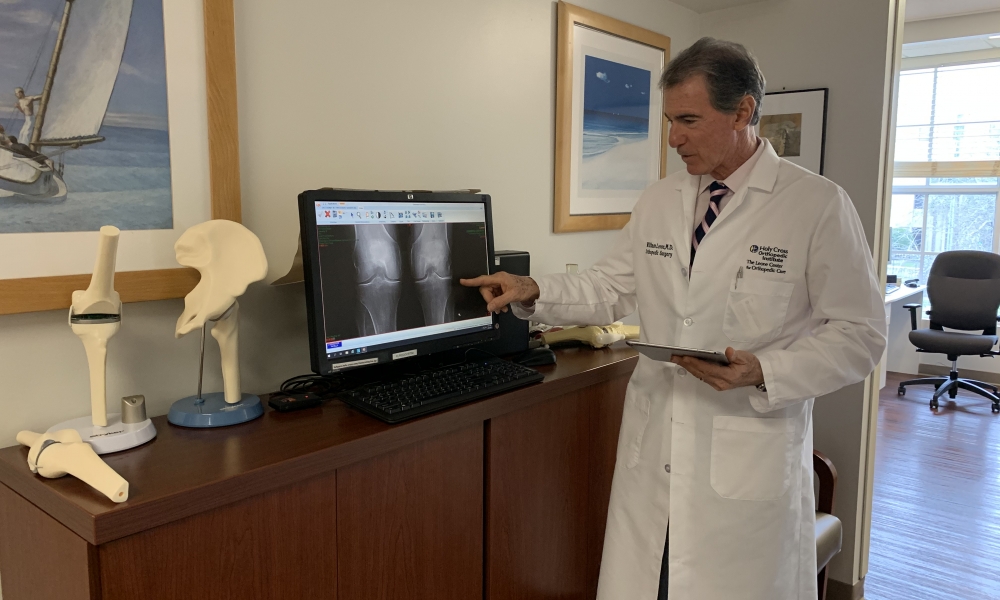
A: Unfortunately, what you’ve shared is all too common. Sadly, many people who undergo TKR are not happy. Our literature reports the number of unhappy TRK patients may be as many as 20 to 30 percent. Still, a much greater percentage of people are happy with their TKRs. So, when the construct is stable, not infected, the soft tissues balanced and knee kinematics are restored, people do really well. But, when one or more of those conditions is not correct, patients are not happy. I suspect you do have an on-going problem with your prosthetic knee joint. In order to resolve it, it must be understood. Often plain X-rays or CTs don’t give us the answer. The character and specifics of symptoms give us valuable clues. Blood studies, looking at inflammatory markers including ESR and CRP, are appropriate. If elevated, fluid is aspirated from the knee for further analysis. Sometimes, I have patients return to the OR so I can analyze their knee movements (kinematics) and balance (inter-compartmental pressures) using an OrthoSensor device. This is a very powerful intra-operative tool, which provides data allowing me to diagnose and then directly address the problem surgically. I recently published a blog article: A Bad Total Knee Is Restored with the Use of an OrthoSensor Device in which I described a patient on whom I recently operated, using this technique to revise his painful and poorly functioning TKR. I think you may find it valuable to read. My advice is to discuss your symptoms and frustrations with your surgeon. If that individual is unable to help you, I suggest you seek opinions with other orthopedic surgeons who have a special interest and skill in treating TKR and revision TKR.
Partial versus Total Knee Replacement
Q: I had a partial knee replacement in Dec 2014 and ended up having a total knee in March 2015. Well, it’s been a year and 4 months and my knee still gives me pain. I cannot sleep. It aches badly. And, there is pain that shoots down it. Not only that, but it is swollen. And, it makes an awful noise. Like it’s loose. Can you help with any info?
A: I’m sorry to learn that you are struggling with your TKR. Converting a partial knee to a total knee does add surgical complexity and I suspect that you are continuing to experience discomfort from less than optimal soft-tissue balancing. Many reasons can cause your symptoms. A further work-up to define the exact etiology of your dissatisfaction and pain is appropriate, which includes trying to rule out an underlying infection. My recommendation would be to return to your surgeon to share your frustration and difficulties and ask for advice. If your surgeon is unable or unavailable to help you, then I would seek out other orthopedic surgeons in your area with a special interest and specialization in complex total knee issues.
The Durability of TKR Prostheses
Q: My right TKR, which is 12 years old, is showing some signs of loosening. My knee will pop occasionally when I rise from a chair. Also, I have small amount of swelling. It feels like a ping pong ball but very soft to the touch. I try to use natural anti-inflammatories like limes and apple cider vinegar. I am 6 foot 5 inches and weigh 260 pounds. I have a goal to lose 30 pounds. I walk 4 days a week vigorously. Also, my business has me on my feet 9-12 hours a day. I would like your input on my expectations of this knee lasting another 5 years or am I unrealistic?
A: I think the expectation that your knee should last another five years is not realistic and possibly detrimental to the final result after your knee revision. Your knee is “talking” to you. I would strongly recommend “listening.” Loosening of the component suggests osteolysis or bone loss. Swelling or fluid suggests irritation and inflammation. You describe instability when arising from a chair. You’re a huge man and very active. As a surgeon who personally wants to deliver the most perfect result possible, I can assure you that it’s easier and more assured when there is less bone and soft-tissue destruction. I would suggest discussing “next steps” with your surgeon.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com. Comments will be answered in as timely a manner as possible.