Poor Results after TKR Due to Infection: Diagnosis and Treatment
For the second of three blog posts about post-surgical complications and unsatisfactory results after total knee replacement (TKR), I will discuss the critical need to rule out infection and if present, how to treat it.
If underlying infection is present, and the infection is not realized preoperatively or intraoperatively, then almost assuredly any further attempt at revision will fail without first treating the infection. As described in more detail in a previous blog post (click here), synovial fluid is aspirated preoperatively from the knee and analyzed for signs of infection. At the time of revision surgery, synovial fluid is collected again and analyzed for total number and percentage of different types of white blood cells, which are indicators if underlying infection (inflammation) is present. Tissue is debrided (removing tissue which appears inflamed, infected or necrotic) from around the prosthetic knee and sent to a pathologist for immediate analysis. The tissue is frozen and the pathologist examines very thin slices (a frozen section) under the microscope to look at cell types and numbers that would be consistent with acute inflammation or infection. If these studies are consistent with infection or infection has been diagnosed preoperatively and confirmed intraoperatively, then the entire prosthesis must be removed. The synovial fluid analysis and the frozen section analysis are communicated to me during the operation. The joint space and exposed bone then are meticulously debrided and irrigated. Then, if possible, a temporary total knee is re-implanted using antibiotic impregnated bone cement (very high concentrations of antibiotics are added to the bone cement during mixing). The antibiotic leaches out of the bone cement during the ensuing weeks and creates a high local concentration. These patients also will require the administration of an intravenous (IV) antibiotic(s) specific for the organism, usually for a six-week period, often followed by continued oral antibiotics. At some point all antibiotics will be stopped, blood studies will be repeated and the knee re-aspirated for synovial fluid analysis and repeat cultures. If no further evidence of infection is found, the patient returns for definitive revision TKR surgery. At this point, the patient has had at least two prior major knee surgeries and many patients also have had surgeries prior to their index TKR. Because supportive knee soft tissue, ligaments and boney structures often are compromised, it can make revision surgeries very challenging.
Occasionally, a decision is made not to remove the entire prosthesis even if infection is present and instead the surgeon will extensively debride the tissues, irrigate and change the tibial plastic insert. However, odds of curing the infection are small, especially if more than two to four weeks have passed since the index surgery and if the infecting organism produces a glycocalyx, a sugar coating that often is referred to as a “slime layer.” This slime layer allows the bacteria to attach itself onto inert surfaces, including the knee prostheses, preventing the antibiotics from doing their job. “Staph” is the most common organism that infects total joints and unfortunately this type of bacteria does produce a slime layer.
One of the advantages of debridement without complete removal of the knee prostheses is that much less surgical dissection is needed. Typically, the patient experiences an easier postoperative recovery and the hope is that no further surgery or second stage-re-implantation is needed. This strategy maybe appropriate if the infection is treated in the early postoperative period (two to four weeks) and with a susceptible organism that does not form a slime layer, or for a patient who is very elderly or infirm and is not a good candidate to undergo two major revision surgeries. In the latter case, it’s important that patients and their families understand that the infection will not be cured, but hopefully suppressed. In the former case, where a patient is infected with a susceptible bacterial organism and is in the early postoperative period, debridement, irrigation and plastic exchange could be performed as an attempt to cure the infection. It should be understood that this treatment ultimately may fail, prompting more surgery for removal and another staged re-implantation.
Many individuals are able to remain active and pain free with a suppressed TKR infection while continuing a regimen of oral antibiotics for life. When I explain this to my patients, I often compare it to someone who is required to take a blood pressure pill or diabetic pill to control that condition for life.
A revision TKR often requires building special prostheses that typically are larger and more complex with stems that are fixed up the femoral canal or down the tibial canal. Metal augments may be added to the backside of the prosthesis that will rest on remaining bone, enabling the surgeon to recreate a more optimal joint line level and a stronger construct. The joint line refers to the position where the femoral component rolls against the tibial component, and if it is too high or too low the joint might not be stable. Occasionally, bone loss is so severe that the surgeon must first implant a metal cone next to remaining living bone and then cement the prosthesis with augments and stem into the cone. The hope is that by bone growing into the cone, it achieves stability.
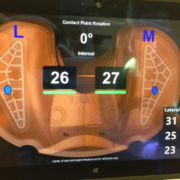
In the third and final post of this series, I will discuss how I use a groundbreaking sensor technology when revising a TKR.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.