Using Kinematic Sensor Technology for Revision Total Knee Replacement (TKR)
In my previous blog about TKRs that look good but feel bad, I discussed how approximately 20 percent of TKR replacement surgery patients are not happy with their results. Occasionally, even when a TKR “looks good on paper,” more surgery is required to correct and improve the existing outcome. If TKR revision truly is necessary, then the specific reason for the failure must be understood fully before it can be corrected. Often, there is more than one mechanical problem.
Some unhappy TKR patients come to The Leone Center for Orthopedic Care who already had workups to explore the etiology of their complaints, but no specific correctible cause or causes were diagnosed. Typically when they present to me, they are frustrated and have seen multiple other surgeons, including the surgeon who implanted the TKR, and none have been able to clearly define why they are doing poorly or outline a plan to improve the situation.
For example, the leg may be satisfactorily aligned, the incision might appear healed and unremarkable, and the range of motion may or may not be satisfactory. Clinically, the knee might not appear infected and often I’m not given a history that suggests infection. X-rays may also appear satisfactory. Often, I’m also told that the patient has had many months of extensive physical therapy following TKR. This patient falls into the “Looks Good But Feels Bad” syndrome. Unfortunately, it is not uncommon.
A proper workup for a painful TKR focuses on three critical conditions that must be combined to recreate a stable, pain-free TKR with a good result. The mechanical axis must be restored, the soft tissues must be balanced throughout the range of motion and normal knee kinematics re-created. It is very difficult to accomplish these conditions consistently, particularly with some pathology and deformities.
I address these goals by using two different computer systems, which has vastly improved the consistency and results my patients achieve after TKR. These computers provide data and measurements that are more accurate and reproducible as well as improve my decision-making during surgery. By using these computer systems, I’m much more aware of how subtle changes in implant position, boney resection and the loading pressures experienced by the surrounding ligamentous sleeve vastly effect the knee’s final balance and kinematics. This greatly enhances the final result.
Typically, surgeons attempt to optimally rotate the tibial component to match the femoral component by the “looking and feeling” method of sizing up the anatomic features or landmarks on the bone. Many times, the precise location of these landmarks is difficult to define or feel, especially in a deformed and arthritic knee, and this leads to a less-than-desired accuracy. Patella tracking also is majorly affected by femoral rotation.
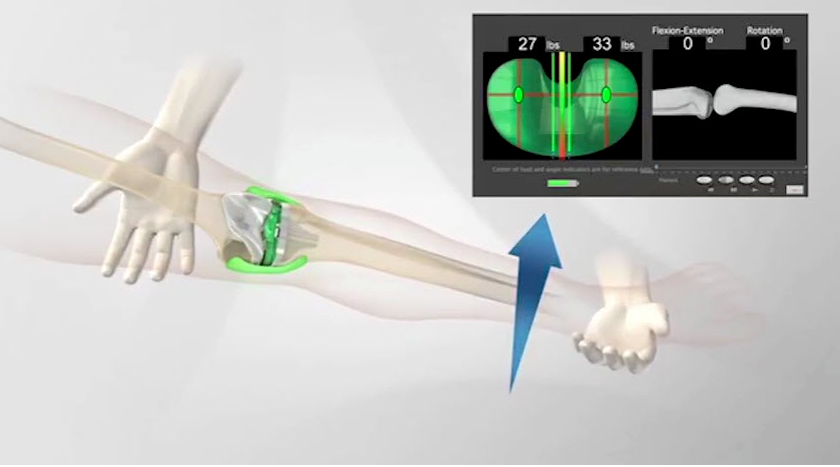
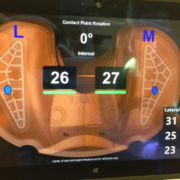
The OrthoSensor device is a trial tibial insert with an embedded microcomputer chip and pressure pads. When placed between the femoral and tibial components, it relays pressure measurements and the location of pressure occurring in the inside and outside compartments of the knee. This information is displayed via radio frequency technology on a monitor in my operating room. I can use this data to optimally rotate the tibial component to contact the femoral component. Once the components are congruent (or perfectly rotated and lined up), I assess and fine-tune the balancing in extension and throughout the range of motion. Frequently, by interpreting the data I will see the need to release a specific tight band or to slightly refine the bony cuts. I’m also able to assess knee kinematics to confirm that the knee is rotating and pivoting on the medial compartment during extension and flexion. The information now displayed on the monitor may direct a release of tight bands within the posterior cruciate ligament (PCL).
For some people who come to me with knees that “Look Good, but Feel Bad” and need revision surgery, I have been able to use this technology to diagnosis subtle rotational, balance and/or alignment problems, which I might not have appreciated just by sight or feel, and then direct specific treatment to correct the problem. I like to compare this scenario to a modern day car mechanic who will diagnose a car problem by simply plugging into a computer. So, why can’t we “plug” a computer into an artificial knee which is not working optimally to help figure out what is wrong so we can correct it? Now, we can.
In some patients, using this technology has resulted in considerably less surgery to correct their problems. For example, revising only one of the major components (tibia tray or femur) and not both. Often, a revision knee surgery is approached with a “start over” or “change everything” mentality because the exact cause of the failure is not crystal clear. It’s far more elegant and less invasive if the problem/problems truly can be diagnosed and solved with less surgery to deliver an excellent result.
In many revision TKR surgeries, there is extensive bony and/or soft tissue destruction. Rather than using standard total knee components, I reconstruct with total knee components that are designed specifically for the revision scenario. Typically, they create more constraint (mechanical interlock) between the femoral and tibial components. The increased constraint results in more controlled movement and substitutes for soft tissues that no longer are able to do their job.
These specialized revision components allow for the addition of modular augments and stems. The augments allow me to customize the components to maximize contact with the remaining host bone and the stems help off-load the increased forces resulting from more constraint and less supportive bone. Even in these situations, I still have found it very valuable to use the OrthoSensor to optimize rotation and confirm load balancing.
I also have seen patients who have done poorly after TKR, whose preoperative workups were not revealing, and at time of surgery component position, alignment and balance all seemed very acceptable. Occasionally, the tissues that envelope the total knee and define the joint space don’t appear healthy and I discover an abnormal tissue reaction secondary to metal sensitivity.
Most total knee prostheses are made with cobalt and chromium. Nickel might also be a constituent metal. Some people develop a hypersensitivity to one or more of these heavy metals and develop symptoms. Symptoms can manifest themselves locally (in the knee) or systemically (throughout the body). Unfortunately, preoperative skin and serum (blood) testing for heavy metals has not translated into a strong and reliable predictor for these hypersensitivities and reactions. Historically, an individual with multiple allergies and/or the inability to wear costume jewelry may be susceptible. This relationship is not absolute. It is critical to go into surgery with a high index of suspension and be prepared to remove the entire total knee and replace it with another made of different metals.
Textbooks include chapters written about the painful total knee, however most patients do spectacularly after TKR. I believe by using the better tools, technologies and insights we have today, the percentage of individuals who fall into this group of “unhappy patients” will grow smaller and that many can be helped and ultimately become part of the group that has done so well.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.