Postoperative Care: What to Expect after Hip and Knee Replacement Surgery
Much of the content on my blog explores the signs and causes of hip and knee degeneration as well as how to decide if and what type of hip or knee replacement surgery is right for you. In this blog, I will discuss what to expect after surgery, from the recovery room to postoperative home care and rehabilitation.
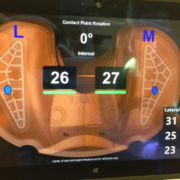
Both hip and knee replacement surgical techniques have greatly advanced, allowing surgeons to perform less-invasive and more precise procedures. These two factors alone facilitate a faster recovery process. Also, the sterile conditions under which I perform these surgeries, including body exhaust suits worn by me and my team, meticulous handling of tissues, and a comprehensive regimen of antibiotics, have vastly diminished the risk of postoperative infection.
In a previous blog, Managing Postoperative Pain, I outlined in detail the multimodal strategy I use to anticipate and manage my patients’ postoperative pain. Managing pain eases both the mental and physical effects of surgery and allows patients to get back on their feet more quickly. Our goal and strategy are to minimize and preempt pain by “staying ahead of the pain curve.” Although managing postoperative pain actually begins prior to surgery, medications also are administered in the operating room and continue postoperatively. Partial or total knee replacement patients also get an adductor nerve block placed before their procedure starts and before nerves are stimulated. During surgery, a combination of three medicines from different drug classes is injected into the surgical area which further reduces early postoperative pain.
Most of my patients receive a regional or spinal anesthetic. This creates temporary numbness and paralysis below their belly button. Patients sleep completely and comfortably throughout the procedure. Importantly they do not require intubation (placing a breathing tube down their throat) because they breathe on their own and require fewer drugs than when general anesthesia is used. Patients also tend to bleed less with spinal anesthesia. Because their paralysis slowly wears off after a couple of hours, any pain they may have is more easily titrated and controlled. Prior to even making an incision, my patient receives an IV steroid which helps down-regulate pain and tranexamic acid which decreases bleeding during the operation and post-operatively. IV antibiotics are also given prior to making an incision.
Once in the recovery room, I prescribe a combination of Intravenous (IV) NSAIDs and Tylenol. While narcotics are often given, the dose required is much less than what was given historically, therefore minimizing complications that narcotics can cause such as nausea and confusion. Many patients do not require any narcotics.
Nearly all my patients are fully alert and begin walking just a couple of hours after their surgery. This is truly wonderful and remarkable, particularly considering the slower pace of post-op rehab just several years ago. Every patient goes into surgery with a preoperative plan. This has been a huge confidence builder which has resulted in faster and more predictable rehab. For most patients, their plan is to go home later the day of their surgery. For others, it might be to stay one or two nights on our orthopedic specialty floor before going home. Occasionally more extended rehabilitation is necessary and arrangements are made for transfer to another facility after discharge from Holy Cross Health. We help every patient create their own plan, even if it needs to be changed.
Physical and occupational therapists review exercises including getting in and out of bed, stair climbing, and using a walker. Part of each patients’ discharge plan is arrangements for physical therapy once home, and already having any medicines including narcotics if appropriate before going home. Also, have any equipment such as a walker or cane that you might need waiting for you. All discharge information is written down for you, including having a post-operative appointment for suture removal two weeks after surgery, the specific agency who will be providing the physical therapist, home exercises for you to do, and specific instructions on taking pain meds. This is “our recipe” that has resulted in a smoother, more confident and faster recovery. Also, a happier patient who has a better experience.
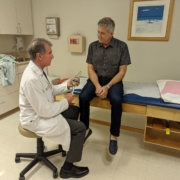
Our goal at The Leone Center for Orthopedic Care is to combine leading-edge technology with good old-fashioned care where the doctor-patient relationship is as important as the treatment. In my experience, patients who go into surgery prepared and knowing what to expect, recover much more quickly. And that is our mission, to restore quality of life by making every step count.








do you accept Human Gold Plus Insurance?
Hi Stan,
Dr. Leone has opted out of Medicare since October of 2009’. If you would like to come in to see Dr. Leone, his fee is $250 and includes X-rays. If it’s determined that they need a hip or knee replacement, Dr. Leone’s fee would be $5,500. The initial consultation fee would be deducted from the surgery fee, and all office visits for 90 days after the surgery is included in the surgery fee. Then, every year or two you would come back in for a follow up visit, which is then charged at a reduced rate of $150.00 including the X-rays. Everything else that may be associated with your surgery; “hospitalization, anesthesia, rehab and any medical equipment that may be necessary”, would all be covered by their Humana Gold plan. Just Dr. Leone’s fee is an out of pocket expense.
Thank You,
The Leone Center for Orthopedic Care Staff
Very informative post, and great timing to find this as my mother is having a hip replacement surgery next week. Thanks for sharing!
I require narcotic pain meds for severe pain caused by my other medical conditions and hip pain. Will I be given the narcotics after hip replacement while in the hospital and while in a rehab facility and for use later in my home?
Hi Jim,
If you already require narcotics and use them on a regular basis, then your body has built up a tolerance. What this means is that post-operatively you will need your baseline medications as well as additional pain medications to be comfortable. Weaning off all narcotics may be an ultimate goal, but decreasing or eliminating narcotics in the post-operative course simply is not appropriate. Because of other medications and modalities I use to combat post-operative pain, I do find that people who are addicted to narcotics still require far less medications than I’ve had to use in the past due to the multimodal regime I use now.
Thank you,
Dr Leone
This blog is incredible. Very informative and gives me hope that, as a single mother, I won’t be left on my own during recovery. Looking forward to meeting with Dr. Leone.
I would like to have advice for me ,to help a dear close friends that the husband is having hip and knee surgery done at the same time.he has ,ms.he will later on have the opposite done.what can I do to help the wife ,to help her husband have an easier recovery time.he has been in so much pain for so many years ,I just want to help him to rest ,eat ,sect.I want to really help in someway.thank you,have a good day.
Dear Rrena,
The family or primary caretaker often does feel a tremendous amount of anxiety and pressure when a loved one is about to undergo surgery. It’s been my experience that when the family or caretaker, as well as the patient, are directly involved in the preoperative education process, then everyone has a better experience. Knowledge is power. When one knows what to expect and what the plan is, it results in much less anxiety.
Your friend needs to feel enabled and that she’s not being put in a vulnerable position that she’s not comfortable with. I would encourage her to write down all her questions and concerns and then address each with the surgeon or his/her “team.” In the hospital, there also will be team to address concerns and help plan for hospital discharge and post- hospital-stay patient care and therapy. She needs to feel assured that her husband will not be discharged until a safe and acceptable plan has been agreed upon. She needs to know that both of them will have the help needed once he is home.
You can help your friend be encouraging her to be involved in the preoperative process to understand the plan. If he will require going to another facility after his surgery, she can find out from his insurance company which facilities will be available to him and then visit those facilities ahead of time so that they can make a more informed decision. You then can help your friend by standing by her and supporting her.
I wish you, your friend and her husband all the best.
Dr. William Leone