Wonderfully, the vast majority of patients who have a hip or knee replacement, walk just hours after surgery and go home later that same day. When I first started my practice, patients were admitted the day prior to their surgery and stayed for a week or more, and many would be then discharged to a rehab facility. This is in contrast to just a few years ago when most patients stayed in the hospital over night or even a few days after their surgery. Every year the time period from surgery to discharge and return to full activities has gotten shorter and shorter because we’ve gotten better. I tell my patients that what has changed the most in my practice is how much faster and seemingly easier patients get well and return to their full active lives.
With the ongoing Covid pandemic, most patients who previously stayed overnight, now want to go home the afternoon of their surgery. I’m happy to report that patients are doing great, they’re happy and complications are even less. It’s become the “new norm”.
I attribute this to better preparation, surgery and after care:
Patients are going into their surgery better prepared. When someone knows what to expect, there is less anxiety and they get well faster. I believe education is power. I see this over and over. We ask our patients to do some simple strengthening exercises before their surgery, which are the same exercises they’re ask to do after surgery. This preoperative conditioning makes the postoperative course easier and the patient is more confident. We help our patients create a plan for “after surgery”. Having a plan, even if it needs to be changed, relieves anxiety and people get well faster. They are prepared mentally and physically. What I see is patients walking sooner and without a limp, driving, and returning to their normal work, family and recreational lives sooner. Typically, when a patient returns for their routine 6-week postoperative visit, the majority are doing so well that I won’t even see them again for several years.
We are definitely doing a better job during surgery. Both our surgical and anesthetic techniques have never been more refined. Surgically, we’ve developed much more exacting methods with minimally invasive techniques. These improvements have resulted in less soft tissue trauma and bleeding with a more anatomical and stronger repair. Respected and time tested hip and knee systems have been further expanded resulting in our ability to choose from a huge inventory of models and sizes, allowing me to “build a construct” which best fits that individual and creates optimal hip or knee mechanics. The wear characteristics of our modern-day knee and hip bearing surfaces (the part of the prosthesis that is actually moving against each other) are a magnitude (x10) better than early generations. This is translating into much longer lasting prostheses, even in super active individuals.
Patients are only better off going home the day of their surgery if they are comfortable (that is, not in pain), independently mobile (certainly we can’t expect a spouse or significant other to lift them), and are not experiencing complications like nausea, vomiting, urinary retention, or confusion.
In earlier blog articles I have discussed my strategy of preempting pain with our multimodal pain management regime. This starts with prescribing medicines before surgery and after surgery, taking a number of other medicines from different drug classes on a schedule. This results in an additive effect with even more profound pain prevention and relief. While narcotics are part of the mix, they are not emphasized. Historically, narcotics were the central pillar to control postoperative pain. During surgery, I inject a “cocktail” of different meds into the tissues surrounding the hip or knee replacement as well as an adductor nerve block for knees.
The Anesthesiologist is also doing a better job during the procedure. That individual who is taking care of you during the procedure and administering the anesthesia is a critical and important member of our team. There has been a clear trend and recognition in our literature, that regional or spinal anesthesia has a number of advantages over general anesthesia when performing a hip or knee replacement surgery.
I am now also seeing a trend returning to general anesthesia for out-patient (patients who will go home the day of their surgery) total joint replacement. This is because administering a general anesthetic is faster, often more predictable, and the patients wakes up quickly when the anesthetics gases are stopped. Hence, it is more efficient and better fits an outpatient surgical center, volume-based model with total joint patients leaving same day.
Having a smooth intraoperative course, a smooth recovery and no reported complications can be accomplished with both Spinal and General anesthesia. There are some patients who have conditions which would clearly favor either a spine anesthetic or a general anesthetic, but these are the exception. Administering a spinal anesthetic is a technical skill, like surgery that requires finesse and practice, especially when the patient is elderly with spinal arthritis and deformity or in patients who have had prior spinal surgery. I believe the advantages that spinal or regional anesthesia offer are important and, in my experience, still fit into an outpatient total joint model.
A big advantage of Spinal vs. General anesthesia is that patients typically require less drugs to remain anesthetized including less narcotics. This is a major reason why more patients after spinal anesthesia seem to feel “more normal” sooner than after a general. Eliminating or greatly diminishing our use of narcotics has wonderfully decreased post op complications like confusion, problems with breathing and constipation. Inhalational gases and other drugs used for general anesthesia can also leave some patients mildly confused after surgery. Some of my elderly patients or their doctors express concern about this and specifically request spinal or regional anesthesia for this reason.
Another advantage of spinal is that patients tend to wake up “smoother and slower”. The spinal anesthetic creates a temporary paralysis of the lower body but does not affect one’s ability to breathe on their own, speak and be fully present during surgery if that is the desire. Most patients (and their surgeons) want to sleep and not remember anything until after surgery and they are in the recovery room. Sleep is induced after the spinal is placed by administering a drug called propofol. It is a short acting medicine given intravenously that induces sleep and amnesia. It’s the same drug used routinely when someone has a colonoscopy and other short procedures. A different drug called versed is administered before the spinal and acts like a short acting valium to relax and also provides amnesia, so the patients doesn’t even remember having the spinal block placed. When the surgical procedure is complete, the propofol is stopped and soon after the patient awakes, but without pain because the spinal block is still active. As the spinal wears off, the patient can again actively move their lower legs. Surgical pain may develop slowly which is treated. This tends to be gradual and narcotics are more easily avoided or minimized.
When the inhalational gases used to induce general anesthesia are turned off, the patient awakes, but now with immediate postsurgical pain. Pain meds are again administered to treat postoperative pain but now more emergently and possibly in higher doses and using narcotics.
Another advantage of spine vs. general anesthesia is that with spinal anesthesia the patients’ mouth and neck are not manipulated. General anesthesia requires controlling the airway. Sometimes a breathing tube (endotracheal tube) is inserted into the trachea and temporary paralysis is induced so the patient does not breathe on their own. Some patients complain of a sore throat after. Patients who receive a spinal anesthesia breathe on their own because their diaphragm is not paralyzed and their airway is not manipulated.
The incidence of DVT or a blood clot developing in the lower extremities may also be less with regional anesthesia vs. general. This is partially because the patient maintains more natural muscular tone and movement throughout the procedure (not paralyzed) with a spinal anesthesia. Spinal anesthesia also lowers arterial and venous blood pressure resulting in less blood loss and a lesser need for postoperative blood transfusion than general anesthesia.
Spinal anesthesia is clearly preferred in some conditions such as COPD and other conditions with pulmonary compromise. During spinal anesthesia, patients breathe on their own and their diaphragm is not paralyzed. Many physicians and patients also prefer spinal when there is underlying cognitive decline such as dementia or Alzheimer’s disease. Some cervical deformities or a particularly difficult airway also make spinal anesthesia the preferred method for anesthesia.
There are some conditions where general anesthesia is the preferred method of anesthesia such as severe spinal deformity or lumbar spinal fusion. An individual with lower extremity neurologic deficits will often have a general anesthetic rather than a spinal for fear that spinal could be accused of making the condition worse. Certain cardiac conditions such as aortic stenosis make general anesthesia safer. Individuals with bleeding disorders also don’t usually have spinal anesthesia because of concern that the trauma of the needle inserted through the lumbar spinal dura could cause bleeding into the subarachnoid space (the fluid-filled space that surrounds the brain, spinal cord and nerve roots). These individuals are best cared for with a general anesthetic. Occasionally, a spinal anesthetic does not provide a complete block or wears off before the procedure is done. The patient is then administered a general.
A disadvantage of spinal anesthesia is that the urinary bladder is temporarily paralyzed and remains paralyzed until the spinal has worn off. With traditional spinal duration, this was too long a time period for the bladder not to be emptied, so a foley catheter (thin tube inserted into the bladder) is inserted. When patients stayed overnight, this was not a problem. This situation is not optimal for someone going home the same day as their surgery. With a general anesthetic, the bladder is not temporary paralyzed.
Many centers have gone back to administering general for all their patients who undergo a hip or knee replacement, especially in the outpatient setting because it is more efficient. I struggled with this because I did not want to give up the advantages of a regional (spinal) anesthetic.
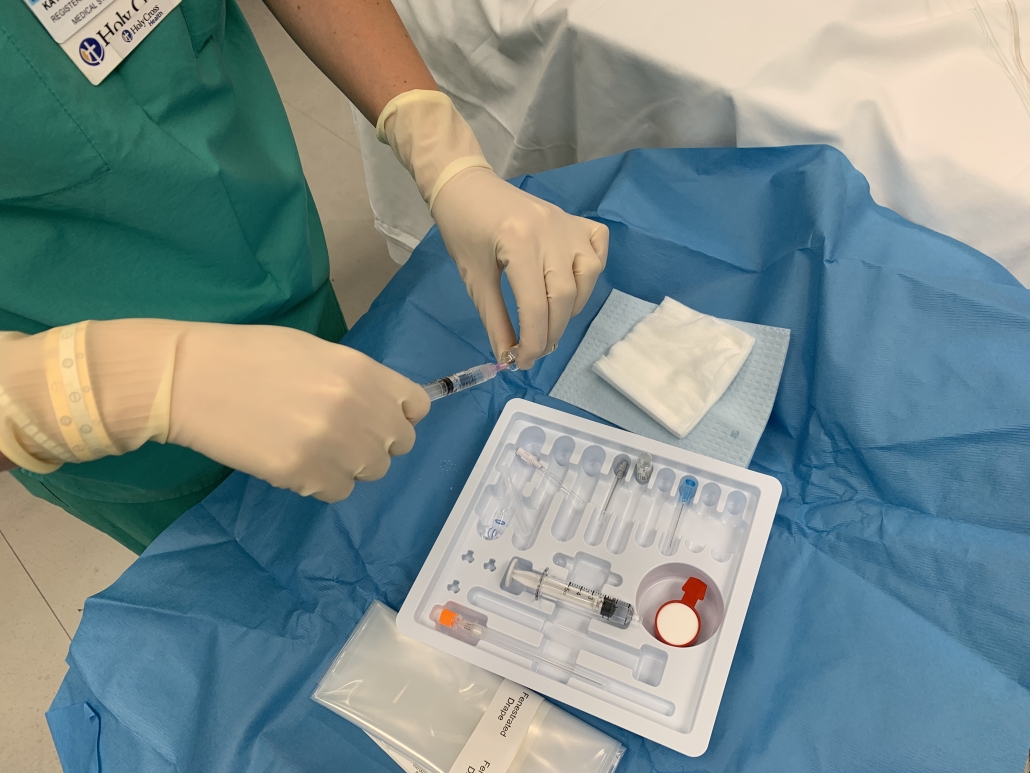
By working with a select team of anesthesiologist and nurse anesthetist at Holy Cross Health, we have modified our spinal technique so that nearly all patients will continue to be offered their choice of spinal anesthesia or general and still go home just hours after surgery. We’ve been affectionately referring to our modification spinal as a “mini spinal”. It is just as effective but lasts a shorter period of time. Patients do not require a foley catheter and can go home later that same day. I consider this the “best of both worlds”.
The amount and type of local anesthesia that is injected into the lumbar spine subarachnoid space determines how long the neurologic blockage (paralysis) will last. The amount selected is based on a patient’s height, age and the estimated time the procedure will take. The shorter a patient, the shorter their lumbar spine subarachnoid space and so the less local anesthetic required. Older individuals tend to metabolize (breakdown) the local anesthetic slower, so less is required. If the total time needed for the procedure is relatively short and the surgical team is “practiced and experienced”, then less local is injected, resulting in a shorter acting block.
The vast majority of my patients continue to receive spinal anesthesia, do not require a foley catheter, walk several hours after their surgery and go home. Our anesthetic teams are using a short acting local anesthetic called Marcaine (Bupivacaine). They are instilling approximately 40% less volume than what was traditionally administered. During surgery, I am unable to tell any difference, other than patients are now routinely fully awake, alert and moving their legs and ready to walk sooner. It does require a practiced and predictable team that works as a team. It’s been very gratifying. I really do feel they’re getting the best of both worlds.
Dr. William A. Leone is head of The Leone Center for Orthopedic Care at Holy Cross Health in Fort Lauderdale, Florida and has earned a reputation as one of the nation’s top orthopedic surgeons. An orthopedic surgeon with extensive experience, his specialty is solving complex hip and knee problems. We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com.