Partial vs. Total Hip Replacement Surgery
“Is A Partial Hip Replacement Right For Me?”
Some patients in need of a hip replacement will ask me if they are candidates for a partial rather than a total hip replacement because it sounds “less invasive.” Unlike the knee (which has three distinct compartments and when one wears out there’s a good chance that only that compartment needs to be replaced), the hip is a single ball (femoral head) and joint socket (acetabulum) and a partial hip replacement often isn’t the optimum choice.
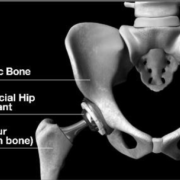
A partial hip replacement (hemiarthroplasty) is the replacement of only the patient’s femoral head. The new prosthetic femoral head (metal ball) then rotates inside the natural boney socket. Our natural socket is covered by hyaline cartilage which acts as a lubricant (decreases friction), a shock absorber, and helps to distribute stress more uniformly within the bone. The new artificial ball placed in the socket is actually against this cartilage. In general, hyaline cartilage doesn’t remain healthy when it moves against an artificial surface rather that hyaline cartilage (i.e. the natural femoral head). Many time this can lead to the breakdown of this special cartilage leading to a compromised result with pain. A total hip involves the replacement of the femoral head and the implanting a prosthetic shell with a plastic liner into the natural socket. With this procedure, the prosthetic femoral head moves within a prosthetic socket.
Bipolar endoprosthesis has small ball which moves within larger ball which moves within patient’s natural socket
Unipolar endoprosthesis has large ball only which moves inside the patient’s own natural socket.
Each procedure has advantages and disadvantages but as a rule, the best results for longevity and consistent pain relief are attained with a total hip replacement.
Fracturing or breaking a hip refers to a break occurring through the upper femur (thigh bone), which often displaces the femoral head. If the fracture occurs within the hip joint capsule, we refer to this as a “femoral neck fracture.” Historically, femoral neck fractures left patients crippled or even caused death due to lack of mobility and all its associated complications. During the 1960s, the one-piece partial hip replacement was introduced. The Austin Moore and Thompson are classic examples of these revolutionary prosthetics. For the first time, physicians could replace a broken femoral head with an artificial one. The stem, which was inserted down through the upper femur bone, was constructed from the same piece of metal as the ball (monoblock). This was a dramatic move forward, saving countless lives and greatly improving mobility and quality of life for many. Although a quantum leap in hip replacement surgery, most patients still had a less than a perfect result, experiencing pain either from the stem not being stable within the femur or the new ball wearing away the natural cartilage.
Today, many people who fracture their femoral necks still are treated with partial hip replacements. Now, almost all prosthetics have a modular head that fits on the stem. A further refinement to the partial hip is the “bipolar” hip replacement. Imagine a standard sized ball, often used in total hip replacement, first being impacted on the new stem and then a bigger ball inserted over the smaller ball and placed inside the natural socket. It’s referred to as bipolar because it can move in two planes: between the little ball and the big ball and between the big ball and the natural socket, as opposed to the original “mono-polar” ball.
Usually patients considered good candidates for a partial hip replacement are those who do not have significant underlying arthritis and have healthy acetabular cartilage. This is often the case for someone who has fractured the femoral neck but did not have hip symptoms or hip arthritis prior. One of the main advantages for performing a partial hip rather than a total hip replacement is that partial hips are inherently more stable. Because the balls are larger they are less prone to dislocation. Another indication for a partial hip rather than a total hip is in a patient who in not a good candidate for total hip replacement do to their medical condition. A physician who does very few total hips also may feel more confident is delivering a better and safer result with a partial vs. a total hip.
The main disadvantage in performing a partial hip replacement is that the final results are not as consistently perfect. Without question, the gold standard is the total hip replacement. More and more recent studies are showing better results with total versus partial, even among the “fracture” population.
As a result, I seldom perform partial hip replacements. There are some patients for whom partial hip replacement is the best course of action. For example, I recently operated on an elderly gentleman with Parkinson’s disease who fell fracturing his femoral neck. Prior to his fracture, he had no hip arthritis. For this patient, a partial hip replacement (bipolar) was most appropriate, because he was not very active pre-fracture, had a high probability of future falls and performing less surgery (replacing only his femoral head and not his head and socket) was safer for him. Also, he did not have hip disease or any arthritic symptoms prior to fracturing his hip. Fortunately, he did very well and after a short stay in the hospital was again able to go home with his wife and resume his prior level of independence.
Another much less common indication to use a bipolar hip replacement is when a patient already has had a total hip, but is suffering recurring dislocations. In some cases, I add a bipolar cap over the ball and then place the large ball into the patient’s fixed cup. This creates a “tripolar” construct and has helped me to solve some very difficult instability problems for patients.
Because of the specialty nature of my practice, I occasionally see patients who already have been reconstructed with a partial hip replacement but are still in pain and not doing well. I convert their partial hip to a total hip by implanting a new socket and changing the ball if the stem is satisfactory. These surgeries tend to be very successful.
For patients who are active and have higher lifestyle demands (want to play golf, tennis, walk for exercise, ride a bike, etc.) I perform total hip replacements, even for a fracture without prior disease. The results are consistently more perfect. It’s a fact that the vast majority of patients who come to me with hip problems have degenerative osteoarthritis. Their femoral head and socket have cartilage loss and degeneration, so a partial hip simply is inappropriate.
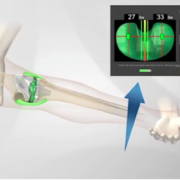
The key to successful joint replacement surgery is having the right surgeon with enough experience to choose the best prosthesis and procedure for you. An orthopedic surgeon who is highly experienced in hip replacement surgery brings valuable expertise and typically has built an experienced team who become your team. Your surgeon also should know from personal experience the most appropriate approach and prosthesis to achieve an optimal, safe, long lasting result.
During my extensive career, I have helped thousands of people from around the world. At The Leone Center for Orthopedic Care, we offer both the latest and most time-tested innovations in joint replacement.
Check out Dr. Leone’s Video Library to watch videos that pertain to your specific questions. You can also find Patient Video and written testimonials.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.







Thanks for sharing this blog with us.This information found very helpful.The Knee Klinik also provides the best treatment for hip replacement.visit us http://www.kneeandjointsurgery.com/
Very nice Information…really helpful..thank you for sharing…