Caring for Patients Who Don’t Heal Optimally After Treatment for Hip Fractures
In my last blog post, I described treatment of hip fractures that occur within the hip joint capsule (intra-capsular) and those that occur outside the capsule (extra-capsular). The strategies for treatment and prognosis often are very different. Fortunately, most people who break hips and are treated surgically do well. However, this isn’t the case for everyone and there are a variety of reasons for poor outcomes. Below I’ve listed some of the more common reasons for continued pain and/or failure after hip fracture repairs:
- Nonunion: the fracture did not heal.
- AVN (avascular necrosis or osteonecrosis): part of the femoral head losses its blood supply and bone dies, later collapsing. This results in joint space destruction with secondary arthritis.
- Post-traumatic arthritis of the hip: the forces that lead to fracture and/or the treatment resulted in injury of articular cartilage, which deteriorates over time.
- Implant problem: pain in the hip and/or thigh from the implanted endoprosthesis.
- Painful hardware: hardware is irritating overlying tissue or sticking into the hip joint socket
- Malunion: the fracture healed but in such a way that pain results with movement due to impingement between the healed bone or hardware and soft tissue. This often is associated with a diminished range of motion.
- Malunion: the fracture healed but with shortening or malrotation of the lower leg.
- Nerve compromise: from trauma that caused the fracture and/or from treatment of the fracture.
- Infection: must always be considered (and will be discussed in a subsequent blog).
Nonunion or fractures that don’t heal:
Previously I explained that the body ultimately must heal broken bones. What a surgeon tries to do is optimize the alignment of the fracture and conditions to encourage healing. The fracture is “reduced” which means we position the fracture fragments in as “stable” and close to “anatomic” position as possible. The fracture fragments then are held in that position by inserting metal hardware (typically screws, plates, cables or a rod). IV antibiotics are delivered to the tissue and hopefully prevent infection. Red blood cells (RBC) carry oxygen to tissues and bone (a living tissue) which must stay alive and viable to heal. The RBC level is anticipated to drop after a fracture and subsequent surgery. Sometimes the drop is so severe that a blood transfusion is necessary to increase the RBC level. Many patients who fracture hips are nutritionally compromised, including over-weight patients. This greatly inhibits the body’s ability to heal the fracture, fight off infection and increases the risk of other potential complications. Diet augmentation with certain foods and nutritional supplements may be necessary. The surgeon will mobilize the patient after surgery but might instruct the patient not to put full weight on the leg until the fracture shows early healing.
Despite all these strategies, some fractures simply don’t heal. Depending on the type of fracture and its fixation, the physician and patient may ultimately realize that simply “giving it more time” will not result in satisfactory healing. More surgery may be recommended, which could include the removal of the hardware and performing a total hip replacement (THR). However, if the call is made to try again to get the fracture to heal, then the hardware would need to be removed, augmented or completely replaced.
The fracture site often is bone grafted, a process where bone is taken from one part of the body and placed in another part to promote healing. Although it’s dead bone being transported from one location to another, our bodies have the ability to grow blood vessels into this dead bone graft and over time convert it into living bone. If the bone is taken directly from the patient, it’s called an autologous bone graft. If it is taken from a donor, it’s called an allograft bone graft. Other biologic materials can be added to promote healing. Sometimes, the act of implanting a new intramedullary nail will create wonderful bone graft simply from femur preparation for that new nail.
If a nonunion of the fracture site develops, and a decision is made not to attempt further repair, the hardware will need to be removed and a prosthetic hip implanted. The empty holes left in the bone by removal of the hardware weaken the bone (stress risers) and could lead to a new fracture.
The femoral stem that is chosen is often longer than a standard primary hip stem, so that it will extend well past the area of nonunion and any empty holes where the screws were removed. Typically in this situation, I place an acetabular component as well as reconstruct the femur because a THR produces the most consistent, best results. I will bone graft the nonunion site and even occasionally reinforce the nonunion site with a new metal plate, screws, cables or even a bone plate to further stabilize the fracture site.
Avascular Necrosis (AVN): when the femoral head collapses:
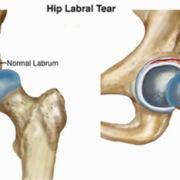
The blood supply to the femoral head is precarious. Frequently, a fracture through the femoral neck can destroy the femoral head’s blood supply, and when deprived of oxygen the head dies.
Blood vessels grow into the areas of dead bone as the body tries to heal itself through a process called “creeping substitution,” where dead bone is removed and new, immature living bone replaces it and eventually matures. When the bone is immature, the head is most vulnerable. If the area of the femoral head that died is in a critical weight bearing position or is a large percentage of the head, then it will begin to collapse because the immature bone is not strong enough. Because this collapsing process can be delayed by as much as 12 to 18 months after the fracture and surgery, it can be particularly devastating to a patient who initially did well but later develops symptoms and evidence of collapse.
Although this is more common following a femoral neck fracture, it also can occur after treatment for an intertroch or subtroch fracture and often is related to the large screw that was placed within the femoral head.
X-rays of the hip may show a subtle lucency or dark line underneath the white outline of the femoral head (subchondral border), called a “crescent sign.” MRI scans demonstrate the condition even earlier than plain X-rays and are very valuable in cases that are difficult to diagnose. The hardware, which is still in the head, may lessen the MRI’s sensitivity to clearly delineate the area of dead bone. New MARS (metal artifact reducing sequences) MRIs help with this problem. A high index of suspicion is important to make this diagnosis, especially in early cases.
A THR is the common treatment for femoral head AVN following a fracture. For a very young person, another attempt may be made to salvage the femoral head by stopping the progression of head collapse and promoting healing by removing the hardware and bone grafting the dead area. New protocols are being developed that add stem cells and PRP with the bone graft, although this is not a common practice.
Post traumatic arthritis of the hip after fracture:
In the previous blog I described the tremendous forces required to break bone, especially in a young person with healthy bones. While the force did result in the broken bones and tissue tearing, it might also have damaged the cartilage that covers the femoral head and socket. Hyaline cartilage is the specialized cartilage that covers the femoral head and the interior of the acetabulum to reduce friction and distribute weight-bearing forces more evenly. This specialized cartilage does not have a blood supply and does not repair itself when injured. When this specialized cartilage is traumatized, it heals with fibrous tissue, not new hyaline cartilage. Over time, fluid within the hyaline cartilage decreases and the cartilage progressively degrades. This degradation process can start immediately after the trauma and slowly deteriorate for years before it causes arthritic symptoms. Also, after a hip fracture, the relationship between the femoral head and the acetabulum may have changed due to the position in which the fracture healed. This too can lead to abnormal cartilage wear and arthritis. Sometimes, cartilage is injured when hardware is implanted or sticks into the joint from undesirable fracture collapse, called “cut out,” because the hardware literally cuts out of the bone.
The bottom line is some people who break their hips later develop symptoms from damage sustained to the joint surface, called post-traumatic arthritis. This can occur soon after the injury and treatment or many years later. If it does occur, it’s treated by removing the hardware and performing a THR. The surgery may be significantly more difficult than performing a THR on a “virgin” osteoarthritic hip due to difficulty in removing hardware and/or the altered (deformed) shape of the upper femur after fracture collapse and healing. In my experience, patients ultimately do very well.
Pain from hip implant:
I’ve seen a number of patients who broke hips and appropriately were first treated with a prosthesis rather than internal fixation in an attempt to save the hip joint. If these patients still experience pain and inability to resume pre-fracture activities, then an infection must be considered and ruled out. This is a very important consideration and I will discuss it separately in subsequent blog.
A common reason why patients develop pain and inability to resume activity after receiving a monopolar or bipolar endoprosthesis is that the natural hyaline cartilage of the hip socket is compromised or worn away causing the prosthetic ball to rub against the underlying acetabular bone. This can occur almost immediately after the surgery or years later. This is similar to what happens to arthritic hip when both the acetabular and the femoral head subchondral bone are rubbing together. In an arthritic hip, it’s known as a “bone-on-bone” condition. After an endoprosthesis, it’s referred to as “metal-on-bone.” Patients develop similar symptoms of “start-up” pain (the particular pain that occurs when someone first arises from a seated position), pain with weight bearing, walking and certain other movements.
Pain after a monopolar or bipolar partial hip can be caused by excessive tension or pressure on the surrounding hip capsule and soft tissues. Occasionally, the source of pain is from the labrum or hip capsule that becomes invaginated into the native socket leading to entrapment. A fragment of bone or bone cement within the joint also can cause pain. In these cases, by converting the partial hip to a total hip and placing a new fixed cup or acetabular component with a smaller ball predictably resolves the pain and in my experience patients do very well.
The hip stem is implanted down the upper femur with the hope that it becomes stable and one with the skeleton. The surgeon may use bone cement to achieve this or a press fit technique hoping bone will grow into or onto the prosthesis. If the implanted hip stem is not stable it can cause pain, classically in the groin and thigh. If the pain is from stem movement in the upper femur, we would expect the pain to occur with movement and not during rest.
Another potential source of pain is from the end of the stem sticking into the side of the upper femoral cortex rather than being centered in the medullary canal. These patients often present with thigh pain that increases when walking.
Some patients will complain of activity-related thigh pain months after surgery when they did not experience it early on. Many times, this is due to a mismatch in the flexibility between the upper femoral shaft (which has a metal hip stem embedded in the medullary canal) and the femoral shaft just below the hip stem, which does not.
The shaft just below the tip of the stem typically is a lot more flexible than the shaft above, which is stiffer because of the embedded metal hip stem. This condition occurs more commonly with non-cemented hip stems and is more common with some designs than others. Fortunately the thigh pain, often described as a deep muscle ache in the upper front and outer thigh, resolves on its own over time, as the body remodels (the femoral cortex thickens) to equilibrate this transition area. Surgery is very seldom necessary.
I make every effort to explain to my patients what to expect. I advise them to be patient and to “listen” to their bodies and back off or decrease activity when they feel discomfort. I also suggest actives that don’t cause the pain, such as swimming or riding a bike. A heating pad or ice can help as well as over-the-counter NSAIDs.
Pain from the Hardware:
The goal of the hardware is to hold fracture fragments in a stable position until the fracture heals. Once the fracture has healed, the hardware no longer is necessary. Usually, most people aren’t even aware of the hardware, so it’s not removed post-healing because that would require another surgery. However, in a very young person it may be appropriate to remove the hardware after the first year in case future surgery is necessary (commonly done for young athletes), or if joint arthritis develops and ultimately a THR is required.
Compressive loads across the fracture site result in some degree of fracture-fragment movement, which hopefully adds to the compression and fracture stability as it heals. The design of the hardware and how it is implanted facilitates a controlled movement or subsidence. Whether a large hip screw or multiple small, cannulated (hollow) screws are placed across the neck and into the head, as the fracture collapses together the bottom end of the screws will back out of the side of the upper femur.
If these screws protrude enough, the ends can irritate overlying tissue. Some complain of pain with pressure or if they lie on that side. Others describe feeling the overlying tissue move, click, and snap over the ends of the screws. Many times, in spite of these localized symptoms, the fracture heals and the hip function returns, yet some remain unhappy because of these symptoms. Removing the offending hardware can solve the problem, however removing certain types of hardware is much more difficult and destructive than removing others.
Malunion:
Malunion refers to a fracture that healed but in a less-than-desirable position. Most hip fractures that aren’t non-displaced require some degree of reduction and internal fixation to hold the position and they ultimately heal in a position that is not perfectly anatomic. This is to be expected. Usually, in spite of healing in a less-than-true anatomic position, patients functionally do well. Sometimes, however, the resulting position is not acceptable to the patient.
Some patients develop significant leg shortening or rotational changes that can alter their gait and cause potential problems with that leg or other areas of their body, i.e., the back, knee or other leg.
Many people will adjust or accommodate to this change and with time it no longer troubles them. Some improve when adding a shoe insert or shoe build-up on the opposite side. Some ultimately have surgery to correct the rotatory malunion or even a hip replacement which allows both the rotatory problem and the leg shortening to be addressed and corrected.
Nerve Compromise:
Occasionally, a nerve injury occurs during the fracture or treatment. When this occurs, it important to understand the extent of the injury: was the nerve cut, stretched or bruised? A neurologist often assists in defining the exact injury. Occasionally, nerve conduction studies and EMGs (to evaluate the muscles’ electric innervation) will be done. An MRI can be valuable to show if the nerve still is being compressed, potentially from fracture fragments or bone overgrowth. In those cases, surgical exploration of the nerve may be indicated to release scar tissue and any surrounding bone. Depending on which nerve is injured, an ankle brace or a knee brace might be worn until the nerve recovers.
Fortunately, most nerve injuries recover completely or at least partially over time. Typically, nerves continue to recover for 12 to 18 months after injury. Often, an early sign of recovery is an increased burning pain. I reassure patients that this actually is a good sign that the nerve is starting to recover, even though it doesn’t feel like it to them. Medications can relieve pain symptoms, but they don’t hasten the recovery of the nerve.
In my next blog, I will discuss infection, both pre- and post-fracture, prevention and treatment.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.