A Hip Replacement Surgery Q & A
As head of the Leone Center for Orthopedic Care, I often am asked to discuss my specialty: hip and knee replacement surgery. One reporter recently asked me to comment on his five top questions about hip replacement surgery. Since these are questions I often hear from patients, I wanted to share this Q & A on my blog.
1. What are the conditions, illness or symptoms that require hip replacement surgery?
Osteoarthritis is one of the most common causes of hip deterioration and destruction. Other causes include congenital dysplasia, hip dislocation, hip trauma or fracture from an accident, rheumatoid or psoriatic arthritis, avascular necrosis, or childhood and other diseases that cause the hip to deteriorate.
Surgery also may be required when the prosthetic hip from a previous hip replacement fails. This can be due to loosening of the components, periprosthetic bone loss (osteolysis) which can also lead to component loosening, infection, recurrent dislocation, leg length inequality, pain, metal toxicity or fracture. Many of these joints have been operated on multiple times before.
If you are experiencing persistent pain in your hip that will not go away, it’s time to have a conversation with your doctor followed by a thorough examination.
2. How can I benefit from hip replacement surgery?
During my extensive career, I have helped thousands of people from around the world, as the art and science of joint replacement surgery has continuously evolved. THR has proven to be a powerful and predictable way to relieve pain and improve function.
At The Leone Center for Orthopedic Care, we offer you both the latest (SPAIRE Technique) as well as the most time-tested innovations in joint replacement.
First, a diagnosis is made based on your personal history, a thorough physical examination and state-of-the-art imaging. I then choose an implant that is best suited to your medical and lifestyle needs. I perform as minimally invasive surgery as possible, emphasizing precise component positioning, meticulous soft tissue handling and closure. This results in less soft tissue trauma and as rapid a recovery as possible.
The goal of a total hip replacement is to relieve pain, correct any deformity and help you restore your quality of life, with pain-free walking and the ability to resume activities that you enjoy. The vast majority of my patients have excellent outcomes and many return to activities such as tennis, swimming, golfing, bowling, dancing, biking, hiking and skiing.
As with any surgical procedure, there are potential risks. I will discuss with you in detail the specific risks associated with this surgery. Once my patients have fully recovered from surgery, most report that they aren’t even aware that they have had a hip replacement and report no limits with activity or bending. Although I have patients who have returned to full contact sports and distance running, these are the two activities that I discourage.
Hip replacement surgery is not just about restoring mobility; it’s about giving people back a quality of life and the ability to fulfill their dreams and ambitions.
3. Are there positions that a patient needs to avoid after surgery and are there any activities that should be avoided after THR?
Our hope after total hip replacement is that the tissues that surround the new hip joint will heal forming a cocoon or wall of surrounding strong tissue. Our natural hip has a “hip joint capsule”. We referred to this surrounding wall of tissue that develops after THR as a “pseudocapsule”. It’s critically important because it helps mechanically prevent the ball from dislocating from the new socket.
Dislocation is a dreaded complication that can occur after THR. Fortunately, our incidence of hip dislocation is extremely small, especially compared to the historical incidence. The very small incidence of hip dislocation we see today has occurred for a number of reasons.
Material scientists working with surgeons and manufacturers have developed plastics (highly crossed-linked polyethylene) which have far superior wear characteristics than the standard plastics we used 15 plus years ago. Because the wear characteristics of the plastic liners we now use is a magnitude better than first-generation plastic liners, it allows us to use larger size prosthetic heads which mechanically improve range of motion and increase the “jumping distance” required for a hip to actually dislocate. This change in the prostheses used has resulted in a decreased incidence of dislocation.
Our minimally invasive techniques result not just in a smaller incision but more importantly a lesser dissection or exposure when performing the THR. The techniques we now use to repair any tissues which are released, especially the native hip joint capsule and overlying soft tissue structures are also far superior to the techniques used in the past and have further decreased the incidence of post-op dislocation. Currently, the latest approach called the SPAIRE Technique has no hip restrictions/precautions. It’s really amazing.
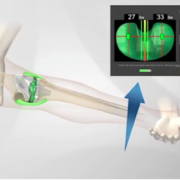
I cannot emphasize enough the importance of placing the components (femoral stem with ball and acetabular shell with plastic liner) in an optimal position in the body. When the components are optimally positioned, the incidence of dislocation is minimized and the chance of improved longevity is improved. The PAL which I will discuss shortly has made a huge difference in my ability to consistently optimizing component position.
Historically patients were taught “hip precautions” after their surgery. These were positions and movements they should avoid so as not to disrupt the soft tissue repair until it healed. Patients were often terrified about making a mistake and their hip dislocating and were never given a clear answer about how long they should exercise these precautions. So much has changed.
I still may ask my patients not to do some things until their hip heals. However, not with the SPAIRE Technique. This means their soft tissues heal and mature. I discuss with every patient the day of their surgery, or the day after, how stable I thought their particular hip was after I completed the reconstructed and tested it. I typically ask my patients not to pull their knee to their chest. I ask them to keep their knees apart when they are bending all the way forward like putting on their shoe or sock. I teach them that if they can “see” the inside of their knee and thigh, then they are fine. The vast majority are encouraged to sleep anyway they want; either side, their back or belly. I ask them to try and keep a regular pillow between their legs for the first six weeks but not to panic if it isn’t there in the morning. Typically, it takes adult tissues 3 or 4 months to fully mature. Clearly, the healing process is well underway by 6 weeks. I emphasize that their hip is stable and they need to get active but use common sense.
Many people after THR forget they’ve had the procedure. I encourage them to fully return to all the activities that they enjoy. That they need to return to a lifestyle that allows them to remain physically fit, happy and balanced. To try and figure out a strategy that encourages hopeful longevity of the joint and isn’t destructive. I discourage extensive long-distance running. Simply banging the pavement for multiple miles doesn’t make sense. I recognize that some patients do, but I don’t encourage it. Likewise, I don’t encourage excessive impact sports like jumping out of airplanes or super heavy weight lifting involving their legs. Over the years, my patients continue to “teach me” what they can and cannot do. I try to fall back on common sense and emphasize that they need to learn to “listen to their bodies”.
4. Do you use the Pelvic Alignment Level only for hip replacements, or can it be used for other procedures?
The PAL was designed specifically for hip replacement surgery. It’s a simple, intuitive surgical device that helps surgeons measure critical variables during the procedure which improves the accuracy and consistency of implant positioning and leg length measurements. The PAL device has a sterile bubble level within an adjustable cradle, similar to the common construction level, which attaches to a small pin anchored in the pelvis. It allows me to correct for pelvic movement and directly measure the cup positioning during cup insertion which results in more accurate cup placement. Also, very importantly, I am able to measure my patient’s leg length before and after total hip reconstruction to see if the leg length has changed and if the changes are optimal and desirable.
5. How long does it take to recover from hip surgery?
My patients are out of bed and starting to walk the day of their surgery and most want to go home the very next day. Everyone tends to be much happier going home. Home is safer than rehabilitative units and I see that patients get well faster when they go home because they do more for themselves.
Going into surgery with more insight and education about what to expect before, during and after surgery ensures a better experience and faster recovery. The pre-op class Holy Cross gives is excellent. My team is wonderful and will help you not only get through the process but also help you create a postoperative plan. Knowing all your options and being organized before surgery again assures the whole process unfolding smoother and with less anxiety.
Walking is the best way to rehabilitate. For many of our patients, we arrange for a home therapist for several weeks. For many having a home therapist improves their confidence and smooths their transition. In general, most patients after THR don’t require a lot of formal therapy although it is available. Most patients report that the deep pain they had before their surgery disappeared almost immediately after their surgery. While there is an incision to heal, the deep pain is gone and they tell me how grateful they are. Most patients quickly return to activities that they enjoy.
Typically, patients return to our office 2 weeks after their surgery. Their suture is removed and we encourage them to start exercising in a pool if available. (Note: patients are given permission to shower as soon as they are home with a special dressing covering their hip incision) The water is a wonderful place to rehab and I think the easiest environment to quickly iron out any remaining limp. Many patients start driving their cars at this point. Most patients have also given up their cane around the two-week mark.
Our patients return 4 weeks later. Most are doing so well they don’t even return to the office for a year for routine follow-up.
Click here to read specifically about Dr. Leone’s SPAIRE Technique. Then enjoy viewing hundreds of grateful patient testimonials.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.