Painful total hip or total knee: Do I have an allergy to the metal prosthesis?
I routinely see patients who are in pain and frustrated with their total hip replacement (THR) or total knee replacement (TKR). Many share with me their belief and fear that their pain is from their body “rejecting” the new hip or new knee due to an allergy to the metal that the prosthesis is made of. While this is possible, it is extremely rare and nearly impossible to prove with a specific study or test, despite claims to the contrary in the lay press and on the internet.
There are a variety of reasons why a patient may suffer a poor result after a hip or knee replacement other than a metal allergy. These common causes must first be “ruled out” (that is, demonstrated not to be the culprit or cause of the poor result) before considering an allergy. An allergic reaction as the underlying cause for a poor result after a THR or a TKR must be considered a “diagnosis of exclusion.” It is the diagnosis made after everything else has been excluded.
Skin patch testing

The vast majority of individuals who have a THR or a TKR are absolutely delighted after their surgery. While the percentage of “satisfied” patients is higher for those patients who had a hip replaced (>90%) compared with those who had their knee replaced (80-85%), in both groups the overwhelming majority are “pleased and grateful.” The group of “less than satisfied” patients in both groups must be better understood. The question that needs to be answered is: What is the difference between the groups that did well and the groups that did not?
The most common causes for a poor result after a THR or TKR are:
- Unrealistic expectations
- Infection
- Mechanical problems including loosening, malposition of the components, and soft tissue imbalance
- Pain that is referred from another source (e.g., the lower back or hip)
- Complex regional pain syndrome
What does “not doing well” mean? I’ve written about “patient expectations” in other articles. If someone goes into surgery with minimal symptoms and/or minimal hip or knee pathology, they are less likely to be happy with their result than someone who has horrible joint pathology and is remarkably symptomatic and disabled. If expectations are not realistic before surgery, then that patient is more likely to be disappointed with their result. At the Leone Center, I discuss with each patient what their expectations are before surgery and what realistic goals are after their surgery.
Metal allergy rash

When someone does not do well after surgery, infection absolutely must be considered and “ruled out.” I have written extensively on this subject. Sometimes it’s easy to diagnose an infection. The joint looks red, hot and is draining. More commonly it’s not so straight forward. An indolent infection (meaning slow growing) can be extremely difficult to diagnose. I explain to my patients that it is vitally important that if an infection is present, it be diagnosed, because if it is missed, almost assuredly any further treatment or surgery will fail. Deciding whether a joint is infected or not begins with a “good history.” I ask if there was a problem with their incision healing after surgery? I inquire if there was prolonged wound drainage or if antibiotics were restarted after the patient was send home. Learning that someone was taken back to the operating room for an infection after their first surgery, historically, is very important and may suggest the infection is still present. A history that someone did well after surgery until they had a procedure like a dental cleaning or developed a medical problem like a urinary tract infection (UTI), diverticulitis, or a skin infection, increases the likelihood that a secondary contamination into the joint occurred and must be thoroughly investigated. If someone is immunosuppressed, either from a condition they have like rheumatoid or diabetes or from medicines they’re taking such as steroids, some chemotherapeutic drugs or “biologics” used to treat autoimmune diseases, the probability that a hematogenous (blood born) contamination of a THR or TKR is more likely and needs to be ruled out.
Obtaining blood work that looks specifically at two inflammatory markers (ESR and CRP) is an important screening test. While these blood studies are not specific to infection, they tend to be sensitive. If an infection is present, one or both values usually are elevated. A number of conditions other than infection can also cause one or both values to be abnormally high. If these value(s) are elevated, I consider this a “red flag.” It makes me take pause and consider if further study such as joint aspiration is indicated. Synovial fluid aspirated from the hip or knee is analyzed under the microscope counting the type and number of different cells as well as if crystals are present. This synovial fluid analysis is a powerful test in helping us better determine if infection is present.
Aspirated synovial fluid is also sent for culture. If bacteria or a fungus grows in this culture, it is strong evidence that the joint is infected. Unfortunately, many times even when the fluid appears grossly infected, the cultures fail to grow an organism(s). This aspirated synovial fluid is also sent for a for a Synovasure test that looks at a specific antibacterial peptide called Alpha-defensin which is released into the synovial fluid in the presence of infection. The Synovasure test has a very high sensitivity (97%) and specificity (96%) and is proving to be a game changer in our ability to now diagnosis infection.
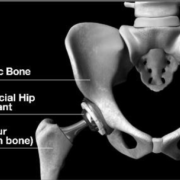
Mechanical problems also account for poor results after a THR or TKR and are a much more common than an allergy to the prosthesis. The components that make up the TKR or THR must be precisely positioned and rigidly fixed to the body if the joint is to function optimally and without pain. If a component(s) is loose, then pain and instability with activity is often experienced such as walking or getting up from a seated position. If the components are not optimally positioned, then soft tissue can be irritated leading to a poor result with pain. If the components are not optimally related to each other, then the natural motion of that joint is not restored which can result in pain, instability, dislocation, and accelerated wear. Some patients complain that one leg feels longer or shorter than the other after a hip or knee replacement and this too can result in an unhappy patient with a poor result. All of these conditions are far more common than an allergy and must be explored and “ruled out” before concluding an allergy is the underlying culprit. In order to convert a poor result into a good one, the etiology of the poor result must be clearly understood and specific problem corrected. Often there are several underlying problems leading to the poor result and all must be corrected.

Pictured above is an image of a modular neck with corrosion from a “recalled hip stem” that I revised. One can see gross black corrosion products which created local tissue destruction and systemic symptoms including a rash. The black appearing Q-tip is from rubbing it inside of the corroding stem.
A poor result can also occur if the soft tissues that support and surround a THR or a TKR are too tight or too loose or being irritated by the underlying prosthesis. The best and most consistently perfect results are when the components are optimally positioned and related to each other resulting in the supportive soft tissues optimally functioning and loaded throughout the range of motion for that hip or knee joint.
Our knee has a wonderfully complex soft tissue sleeve that supports and guides the movement as the knee flexions and extends while pivoting on the inner compartment. When the knee flexes, the lower leg internally rotates and then during extension, the lower leg externally rotates. If this natural movement is not recreated after the TKR, part of the supportive knee sleeve will be too tight and other parts may be too loose. This is a very common reason why many patients are not happy with their result after a TKR.
Our hip joints also has a supportive soft tissue sleeve but unlike the knee it is not made up of fixed ligaments. After THR, if the supportive soft tissue is too tight, it can result in the operative leg feeling longer than the other leg. Sometimes it can also result in a nerve injury. If the iliopsoas tendon is too tight or is being forced to take a longer course over the new prosthetic cup or ball, some patients will complain of groin pain with active hip flexion. If tissues are too loose, then there may be an increased incidence of hip dislocation or weakness with residual limp.
Pain associated with a THR or TKR can also be referred from another source such as the lower back. A pain associated with a TKR can also be referred from a diseased hip joint. Complex regional pain syndrome is another condition that can result in pain in a hip or knee and while rare, is still more common than pain from an allergy to the metal prosthesis. I’ve listed briefly the more common causes of pain or dissatisfaction associated with a TKR or a THR. These are the “big ones” that need to be “ruled out” before concluding that the poor result is from a metal allergy to the prosthesis. Remember, common things are common. My dad used to tell me, “look for alley cats in the alley, not tigers.”
What about an allergy to the prosthesis?
The association between metal implant failure and allergy is well documented but is unpredictable, poorly understood and is highly debated. The direction of the causation is not clear. What came first? Did the implants fail or function poorly due to a pre-existing metal hypersensitivity or did the sensitization happen secondary to excessive metal release from the implants failing? I suspect both scenarios occur. Unfortunately, thus far our literature has not provided definitive answers. Recognize there is controversy and that an orthopedist, dermatologist and immunologist interpret their literature through a different lens.
There are individuals who develop a true type IV or delayed hypersensitivity reaction (cell mediated response rather than an antibody mediated response) and who develop significant morbidity including loosening of their prosthesis, pseudotumor formation and device failure. They can also develop skin eruptions (rashes and chronic dermatitis) and well as systemic problems effecting multiple organ systems. Our conundrum is predicting who will develop an allergy, how best to diagnosis it and then how to best manage our patient who we believe has developed a true hypersensitivity to their prosthesis.
Orthopedic implants are made from alloys and typically include cobalt chrome, titanium and stainless steel. These alloys are made from a variety of metals which are selected because of their biocompatibility, mechanical properties (strength and flexibility) and resistance to corrosion. Commonly these include nickel, cobalt, chromium, molybdenum, zirconium, iron, and vanadium . A clear relationship has never been demonstrated between an individual who is allergic to a specific metal(s) and their result after a TKR or THR which contains one or more of those metals.
Rash from Nickel allergy

Nickel is the most common metal that is associated with an allergy. I’ve had many patients share with me their concern that they’re allergic to nickel, because they can’t “wear costume or cheap jewelry.” Some report having a positive “skin test” to nickel. Having a positive “skin test” to nickel or other metals does not correlate with how well an individual patient does clinically after a knee or hip replacement which contains one of those metals or how long their prosthesis will last.
Some literature finds that individuals who “report” having an allergy to a specific metal had decreased “functional outcomes” after TKA and poorer scoring of “mental health” after THA, compared to individuals who do not. There is other literature which refutes this. It’s also been reported that individuals who claim to have more than four allergies had decreased improvement and functional outcomes after a TKR or THR compared to those with fewer allergies.
At the Leone Center for Orthopedic Care I carefully consider each patients’ concerns and anxieties when I’m selecting the most appropriate implant, recognizing there is a lack of scientific literature to guide us. Sometimes I can easily select one particular prosthesis over another because it’s made from metals and materials that they don’t report having an allergy to. Psychologically this can be “comforting” by eliminating this worry. Sometimes, however, I can’t because an alternative selection simply isn’t available or would compromise my ability to reconstruct the hip or knee satisfactorily. This is particularly true when revising a hip or knee that has failed. I think this is an important conversation I have with my patient before their surgery.
There also exists confusion and debate regarding who should be tested for metal allergy and what is the most appropriate test. Determining a delayed-type hypersensitivity to metals can be done via two routes: by skin patch testing or through a blood test such as the lymphocyte transformation test (LTT). Skin patch testing is relatively easy to perform, readily available but has shown little value in predicting the clinical outcome and is not recommended as a guide for implant choice. If a patient has a history of being allergic to a specific metal and I can choose a hypoallergenic implant that will not compromise the result I do; but again, this decision is not based on firm science. The LLT is a blood test that is not widely available, is not standardized, has inter-laboratory variability and is often not covered by insurance. I consider the LLT mainly a research tool whose results don’t consistently correlate to how well a particular patient will do clinically. Most dermatologists consider the skin test to be the gold standard for diagnosing a Type IV hypersensitivity. Most orthopedist do not think a relevant correlation exits between patch testing on the skin and likelihood or not of an immunologic response developing in and around the bone–implant interface.
Clearly there are individuals who are allergic to a metal(s) within their total hip or total knee prosthesis. A very small percentage of these people develop symptoms as a result of this allergy. These occur very rarely and are exceeding difficult to truly prove. A diagnosis of “metal allergy to the prosthesis” should only be made when other much more common diagnosis are “ruled out.” If you are concerned you are one of those individuals with a hypersensitivity to your metal prosthesis, I would encourage you to discuss your concerns with your surgeon. Possibly revising the prosthesis to one that does not contain the metal that you are allergic to will help you. If you are concerned you may develop an allergy to a proposed THR or TKR prosthesis, once again, I would encourage you to discuss your concerns with your surgeon. Possibly a different prosthesis can be selected.
Check out Dr. Leone’s Patient Testimonials. These grateful patients make it all worthwhile.
Dr. William A. Leone is head of the Leone Center for Orthopedic Care at Holy Cross Hospital in Fort Lauderdale, Florida and has earned a reputation as one of the nation’s top orthopedic surgeons. An orthopedic surgeon with extensive experience, his specialty is solving complex hip and knee problems. Call 954-489-4575 or visit HolyCrossLeoneCenter.com to schedule a consultation.