New Sensor Enhances Precision Balance During Total Knee Replacement
Multiple studies have reported that the percentage of patients who are completely satisfied after total knee replacement surgery is considerably less than with patients who have had a total hip replacement. A number of studies estimate that 20 percent of patients who have undergone total knee replacement are less than completely satisfied as compared with some 95 percent of patients who are satisfied after total hip replacement surgery.
One of the major reasons is that it is extremely difficult for surgeons to consistently recreate normal knee alignment, balance and kinematics. The knee is much more than a large hinge joint. When a normal knee flexes, the tibia (shin bone) internally rotates around the medial (inside knee) compartment while the lateral femoral condyle (the lower outside end of the thigh bone) moves backward in a controlled fashion and slides off the back of the tibia. This complex motion reverses as the knee extends. During knee extension, the tibia externally rotates and the lateral condyle of the femur moves back onto the outside of the lateral tibial plateau (upper surface of the tibia).
In a normal, well-functioning knee, the alignment of the knee ensures that weight bearing forces are distributed equally between the medial (inside) and lateral (outside) compartments of the joint. This results in the tensions within the soft tissue sleeve, which surround the knee, being nearly equal on both the inside and outside, throughout the knee’s range of motion. The soft tissue sleeve helps to support the knee.
Some people are born with a slight sway back of the knee (recurvatum deformity), which as kids we dubbed as being “double jointed.” Likewise, some people develop a degree of bowleg or knock-knee deformity, which they have had for a lifetime and feels normal to them. These angular deformities create eccentric forces which over time can cause the deformity to worsen and the knee to degenerate. It is important when performing a total knee replacement not to over correct these types of deformity. Many patients are more comfortable if to a small degree these conditions are allowed to remain.
This also helps to explain why some people who have had a knee replaced are not completely pain free, even though their X-ray images show perfect alignment. Many of these folks might have had some degree of angular or sway back deformity before the surgery and they now are not comfortable with a perfectly “straight” leg.
Traditionally, surgeons balance the prosthetic knee by feeling the tension in the ligaments throughout the range of motion. This “art-of-feel-based” decision-making is inconsistent and doesn’t allow the surgeon to recognize subtleties within the soft tissue sleeve, too often resulting in areas that either are too tight or too loose.
Fortunately, new techniques and prostheses continue to be refined for total knee replacement surgery. For a number of years I’ve preformed total knee replacements with the aid of a computer, which has greatly enhanced my ability to realign the limb more accurately. I like to think of this as a GPS in my operating room, because I can see on a computer screen the proposed bone angles and levels which need to be cut in order to create the desired limb alignment. This “real time” imaging allows me to make small adjustments to optimize the final result before any actual bone is resected.
I now have added to my computer-assisted technique by using a new, super high-tech device, being developed in Fort Lauderdale, called the VERASENSE Knee System. This new device contains a microcomputer chip with imbedded sensors that transmits precise information wirelessly to a different monitor in the operating room and makes my “GPS” vision even more powerful.
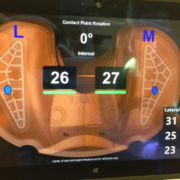
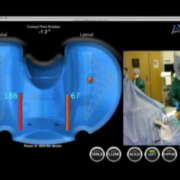
Now, I am able to visualize on a computer screen the exact pressure on either side of the new joint throughout the range of motion. By measuring both the amount and location of the pressure in the medial and lateral compartments of the knee, I know the tension in specific ligaments. Using the VERASENSE Knee System I can optimally rotate the tibial tray in real time to center the forces medially and laterally between the tibia and femur. This step alone often greatly improves the balance of forces on the inside and outside of the knee. I then selectively release specific tight bands within the surrounding soft tissue sleeve using just a standard hypodermic needle, no longer a scalpel, to fine tune the balance of forces. As I move the knee throughout its range of motion, I can visualize the knee’s kinematics on the monitor, confirming stability and that the knee pivots properly around the medial compartment during flexion.
Since using VERASENSE I have gained tremendous new insights regarding how slight changes in component rotation vastly alter the collateral tensions and kinematics in the knee. I’m now also much more selective in releasing only specific bands or fibers which are excessively tight. Simply, it’s much more precise. All of this allows me to create the most optimal positioning of the prosthesis and balancing of the soft tissues for each patient’s individual comfort.
Just last month, I revised a knee that had been implanted by another surgeon. My patient was never happy or comfortable with her new knee and despite extensive therapy she never could fully extend it and her flexion was restricted. After I examined her, I determined that the tension between the medial and lateral compartments was not balanced.
I went into surgery with a plan of how I was going to correct her balance and improve her knee motion, but my plan completely changed when I inserted the VERASENSE. I found that by simply correcting the tibial rotation, the imbalance (which I appreciated before her surgery) disappeared, her knee could now fully extend and flex and optimal kinematics were produced. I ended up performing considerably less surgery with less dissection than I originally had anticipated.
Although her surgery was only several weeks ago, she told me she felt better immediately and was home from the hospital two days after the procedure. I anticipate that she’s going to need much less outpatient physical therapy than she had after her first surgery.
What this means for me as a surgeon is that by combining the VERASENSE with computer navigation, my surgical ability to predictably and optimally perform a total knee replacement is enhanced. This latest computer-assisted technique allows me to construct the best suited knee for each patient’s unique anatomy.
What this means for my patients is a faster recovery time with new knees that feel more natural and work as closely as possible to a normal knee.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.









This article is extremely intriguing. I am a prospective patient for a total knee replacement as determined by my orthopedic surgeon over many visits. I’m functioning generally well currently, but there are times when my knee suffers from over activity and stress, which is painful. I need to know how frequently are these devices used in knee replacement procedures, and how do I find where and who are the surgeons who are skilled in their use? I look forward to your response.
Dear Sheila,
The VeraSense OrthoSensor is produced by a OrthoSensor Inc., Dania Beach, Fla. and trial inserts are being now produced by Stryker, Zimmer, Biomet, and Smith and Nephew for their current total knee systems. DePuy is the one major orthopedic company that has not yet produced trial sensors for its total knee system. This new kinematic technology is presently being launched throughout the U.S. as well as in many other countries around the world. Many centers are using the OrthoSensor but certainly not all. I would suggest discussing this with your surgeon. I would imagine that if you contacted the company and inquired which surgeons in your area use this device and have expertise, OrthoSensor, Inc. would be able to advise you. Honestly, it does take a number of cases before one becomes facile with its use and the information provided. I’m amazed how much more information I get now (as opposed to when I first began using this device) and how that information changes what I do, having used it for several hundred cases.
I wish you a full and excellent recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.