Greater Trochanteric Bursitis: A Common Cause of Hip Pain
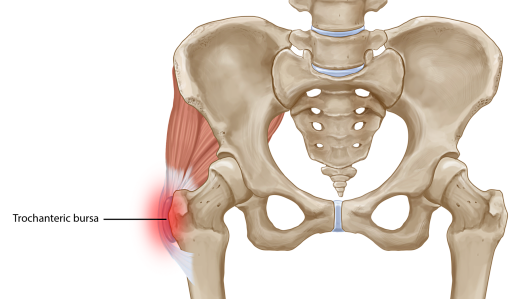
One of the most common sources of hip pain is greater trochanteric bursitis caused by inflammation of the bursa, which is located at the outward curve of the femur (thighbone) where it meets the hip bone. The bursa provides a cushion to reduce friction between the femur’s boney knob and large tendons, and the muscles that run over it and control hip movement. When the bursa sac becomes irritated or inflamed, first it causes pain or tenderness to the outside of the hip and then as symptoms progress this pain can spread down the thigh, to the buttocks, to the groin and/or to the lower back.
Greater trochanteric bursitis often is called the “great mimicker” because symptoms are similar to those of other conditions, including osteoarthritis or lower-back pain. Even though chronic hip tenderness can be the result of a variety of conditions, greater trochanteric bursitis is most often thought to be the result of a damaged tendon or muscle. Bursitis also is more common in women and tends to affect middle-aged or elderly people. As a hip replacement surgeon, I also see many people develop greater trochanteric bursitis caused from an underlying problem with their prosthetic hip joints.
In this blog I will explore the signs, symptoms and causes of trochanteric bursitis, as well as what can be done to treat and prevent it.
The common causes of greater trochanteric bursitis include:
- A hip injury from falling, bumping into something or lying on one side for long periods of time
- Repetitive trauma or overuse which can occur after running, climbing or even standing for long periods of time
- Poor posture, awkward body mechanics, a leg length inequality or a limp all can overstress the tissues in the region of the greater trochanter leading to inflammation and pain.
- Scoliosis, lumbar and sacroiliac joint arthritis, as well as other spinal conditions
- Hip arthritis often presents with greater trochanter bursitis.
- Previous hip surgery, particularly with a lateral approach or hip arthroscopy
- Hip bone spurs or calcium deposits
- A bony fracture or lesion in the upper femur has to be considered and usually can be ruled out with an X-ray. Occasionally, a CT or MRI scan is indicated.
Since I specialize in caring for people with problems specifically related to hip joints, when I examine patients with hip pain, greater trochanteric bursitis is one of the first etiologies I consider. Some of the most common complaints include experiencing hip pain when:
- Pressing on the outside of the hip
- Walking or climbing stairs
- Lying on the side of the painful hip
- Doing activities, including something as ordinary as standing from a seated position, especially after sitting for a long period of time
- Getting out of a car
Many of the patients who come to The Leone Center for Orthopedic Care for a consult do so because they no longer can bear the pain of simple, everyday movements disrupting their quality of life. Some cases of bursitis improve over a few weeks, however if the pain is persistent and you experience any of the following, you should seek a medical consult and treatment:
- Pain that interferes with normal day-to-day activities, particularly if the pain is worsening with time or awakening you from sleep
- Soreness that doesn’t improve despite use of OTC medications such as ibuprofen, as well as resting and ice
- A fever develops or the hip area is red, swollen or feels warm
- If you are concerned that the hip pain may be related to other medical conditions or medications that you take
If greater trochanteric bursitis is diagnosed, your physician should design a treatment plan to meet your goals to relieve pain, inflammation and restore mobility. Initial treatment includes activity modification, rest and ice/heat modalities. If these do not alleviate the symptoms, your doctor may suggest more advanced treatment options such as:
- OTC or prescription anti-inflammatory medicines, such as ibuprofen or naproxen
- Use of corticosteroid injections often mixed with a local analgesic to decrease inflammation and pain
- Physical therapy and exercises to stretch, strengthen and improve range of motion
- Topical treatments including NSAID and steroid creams, as well as patches with NSAIDs and sustained-release local anesthetics
- Some centers are studying treatment with PRP injections.
- Surgery has to be considered, but only as a last resort when all conservative treatments have failed. During my career, I have never operated on anyone specifically to treat a greater trochanteric bursitis.
Because most cases of bursitis are caused by joint overuse or abuse, it is important to listen to your body as the best treatment is prevention. Here are some measures you can take to modify or avoid bursitis:
- If you have any underlying conditions, such as unequal leg length or an arthritic knee or ankle, seek corrective measures such as orthotics, braces or surgery.
- Correct improper posture or sports techniques.
- Begin any physical activities slowly with a “warm-up” and gradually build up the level.
- Avoid repetitive activities, sports or positions that put undue stress on your hips or would exacerbate inflammation.
- Lose weight, if applicable.
- Maintain strength and flexibility of the hip and lower leg muscles; simple walking or walking in a pool will help with this.
- And, it goes without saying, stop any activities if unusual pain occurs.
People are living longer today and enjoying more-active lifestyles well into their 70s, 80s and 90s. While treatments, especially hip and knee replacement surgery, have evolved to keep people moving, taking care of your joints with reasonable expectations also can help you avoid or at least push surgery to a last resort. Today, prevention and treatment both are about restoring more than just mobility, but also lifestyle. Taking care of your joints could help you realize both.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.