Why am I not doing well with my total knee, and when should I consider revision knee surgery?
I’ve written many blog articles detailing problems that can develop after a total hip or total knee replacement, how to diagnose and how to treat. Many of these articles have been wonderfully read and shared. The vast majority of inquiries directed to my website are questions about problems after a total knee replacement. Common queries include: Should my knee still hurt one to two years after knee replacement? What are symptoms of a wrong size knee replacement? Should my knee still hurt, feel stiff or swollen a year after my knee replacement? And many more questions along this theme.
The vast majority of people who have knee replacements are happy with their results. For those people who are happy after their total knee, invariably certain critical surgical conditions were successfully created during their surgery. Unfortunately, when these critical conditions were not satisfied, the result is often less than desirable, and patients can feel pain and instability. It’s estimated that 20% of people who have their knees replaced are not satisfied with their result. I think this is a staggering number, especially considering that over 800,000 Americans undergo knee replacement surgery each year, and this number is increasing every year.
In my practice, I frequently see patients for “second opinions” who are not happy after their total knee replacement and are looking for answers. Most present with a nicely healed incision. Their leg usually looks straight or nicely aligned, their knee has a satisfactory range of motion, and X-ray images show a good quality implant which appears aligned and stable. They’ve invariably visited several other orthopedic surgeons for second opinions but are still without answers. I characterize their knees as “looks good but feel bad”. Sadly, this occurs far too commonly.
Figuring out what is wrong: Unless the etiology of why the knee isn’t functioning optimally and why they are not happy can be determined, treatment can’t be directed at fixing it. The key is figuring out what went wrong. Many patients can be greatly helped when whatever is wrong is corrected.
What are the critical conditions for a successful total knee?
- Optimally realigning the knee by correcting but not overcorrecting any annular deformity that may have developed. If someone has always had some degree of bowleg or knock-kneed deformity, then their soft tissues developed to support their knee in this position. Surgically straightening their leg past this point may not produce the best result.
- Optimally balancing the soft tissue ligamentous sleeve that supports and guides our knee as it moves. Our knee is much more than a “big hinge joint” that only flexes and extends. When our knee flexes, it also pivots around the inner (medial) compartment so the tibia or lower leg bone internally rotates and the back of the femur (posterior femoral condyle) partially falls off the outside (lateral tibial plateau) of the upper tibia. When we straighten or extend our knee, the reverse happens. The tibia externally rotates, pivoting in the medial compartment, and the femur again moves on top of the lateral tibia. Imagine the intricacies within this complex soft tissue sleeve that guides this movement every time we flex or extend our knee.
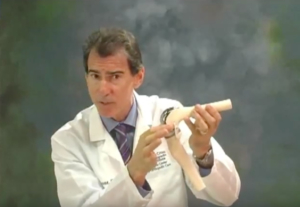
The goal when performing a total knee replacement is to resurface the worn-out surface ends of the femur and tibia, and to rebalance the knee’s ligamentous soft tissue sleeve, so the knee again moves like it did before it developed arthritis. The closer the total knee surgery recreates this normal movement with normal physiological loads or tensions in the ligaments, the better the result. As a surgeon, we love when our patients tell us that they “forget they had a total knee.”
- When this soft tissue sleeve is not balanced (part of the sleeve is too tight, or too loose or deficient), patients complain that their knee does not feel comfortable, or that it feels unstable, especially going down stairs or on uneven surfaces, or feels weak, or that they feel a band-like discomfort, “like it’s twisted.” Some people complain that their knee feels tight and cannot fully extend or flex. Others have discomfort only with activity, while some complain of constant pain. These symptoms are all clues regarding what’s causing the problem and hopefully are a road map for addressing and fixing it. Another critical condition that must be satisfied is that the implanted components must be stable against the bony skeleton, that is, they’re not loose. During activity, a loose component can move against the bone it is positioned against, causing pain. Achieving stable components can be accomplished using bone cement or by coaxing bone to grow into the underneath side of the components. Both methods can work well. One method or the other may be more appropriate for each individual.
- The implanted knee components must also be appropriately sized to recreate the natural relationship and distances between the femur, tibia and patella throughout the range of motion. Components that are too small can lead to soft tissue sleeve laxity and instability. Components that are too large can result in a decreased range of motion with tightness. These patients sometimes complain that their knee feels “over stuffed.” The knee components must also be optimally positioned on the bone. Components that overhang the natural bony contours can irritate tissue and cause pain.
- The components must be optimally positioned or “congruent” relative to each other. When they are not, some patients complain that their knee feels “twisted” or “tight”. Less than optimal congruency can lead to less than optimal tracking of the patella, poor balancing of the soft tissue sleeve and increased wear.
- The knee must not be infected. Infection is often not obvious. Patients rarely present with a fever or chills. Many times, the incision does not look red or feel hot. Seldom is there drainage from the knee. I always ask if there were any problems with their incision healing after surgery, or if they were given a course of antibiotics to treat redness after surgery. If an infection is present, patients often have some level of constant pain (the infection is always active) versus pain only with activity or with certain positions to suggest a mechanical rather than an infectious etiology. It is critical to think about and rule out infection, even if there are no obvious signs. If an infection is missed, any further surgical correction will fail.
- Realistic expectations. Expectations after a knee replacement must be reasonable. Sadly, they often are not. Having a knee that doesn’t swell and hurt after activity is reasonable. Being able to walk pain-free and enjoy even vigorous activities like tennis, pickleball, golf, hiking, swimming, biking, dancing, and other activities is reasonable. It’s probably not reasonable to think that you’ll run marathons or play club soccer, although some patients do, despite my discouraging them. Going into surgery with “reasonable” expectations begins with a conversation between you and your surgeon.
Now what do you do?
If you’ve had your knee replaced and you’re not doing well, it’s critical that you figure out what is wrong. I would encourage you to return to your surgeon and share your concerns. He or she can hopefully help you explore what’s wrong. This probably will include a detailed history, examining your knee and taking new X-rays. It may also include special imaging studies like a CT or MRI. Work-up should include blood work looking at inflammatory markers to rule out infection. Removing fluid from the knee for analysis may also be indicated, especially if the inflammatory markers are elevated.
If you don’t feel you’re getting answers from your surgeon, I would recommend seeking the opinion of another orthopedic surgeon, preferably one who has a special interest and expertise in total knee and revision total knee surgery. If you can figure out what’s wrong, then there is a good chance it can be corrected, and that is a reasonable goal.
If you are struggling after having a total or partial knee replacement, consider scheduling a consultation with Dr. William Leone at the Leone Center for Orthopedic Care at Holy Cross Health in Fort Lauderdale. Dr. Leone is a leader in the field of hip and knee replacement, attracting patients from around the nation and the world. He is renowned for his surgical expertise while providing the highest level of attentive, personalized care in a warm and welcoming environment focused on hip and knee replacement surgery. To schedule an appointment, please call Dr. Leone at 954-489-4575 or visit holycrossleonecenter.com.