Arthroscopic Techniques to Stimulate the Production of Joint Fibrocartilage
In the third blog focusing on biologic strategies to preserve, “heal” or encourage the growth of new joint cartilage, I will describe three arthroscopic techniques that deliberately cause bleeding to stimulate the development of fibrocartilage to form and cover an exposed, arthritic area in the joint. These techniques include drilling, abrasion and, the most recent refinement, microfracture.
As with steroid injections, hyaluronic acid supplementation, and PRP (platelet rich plasma), these methods also have the potential to relieve pain and slow the progressive destruction and loss of hyaline cartilage. Unfortunately, these procedures only offer temporary relief and don’t solve the underlying problem. All three are surgical procedures which typically are preformed arthroscopically.
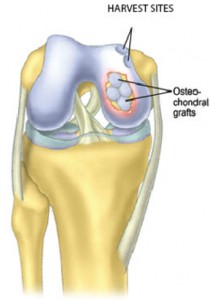
Drilling, abrasion and microfracture all deliberately traumatize an area of subcondral bone (causing it to bleed) that is absent of overlying hyaline cartilage. The goal is for the resulting clot to organize into fibrocartilage. This process takes approximately six weeks to four months. After the surgery, the patient typically is asked to avoid bearing weight for six weeks, by using a walker or crutches, so the clot is not disrupted. The patient may be involved in physical therapy during this period and then after, for strengthening and increasing range of motion.
During arthroscopy, small perforations or fractures are made through the bony base of the small lesions or “craters” where the hyaline cartilage has been destroyed and the underlying supportive bone is exposed. Care is taken to perforate all the way through this layer of bone (subcondral end plate) that normally supports the cartilage in order to induce bleeding. Special multi-potent mesenchymal stem cells are released from the bone marrow, and these cells have the potential to differentiate into varied types of tissues to help organize the clot into the fibrocartilage.
Typically, all of these procedures are limited to cartilage lesions less than 2.5 cm (about an inch). These techniques tend to be less effective in treating older or overweight patients. Many people do enjoy pain relief after these techniques, but the results can be unpredictable both in terms of the amount of pain relief and how long it lasts. Unfortunately, some patients do not do well and report their symptoms accelerating, particularly once they are encouraged to bare full weight on the leg and their activity increases.
These techniques attempt to produce fibrocartilage because the lost, native hyaline cartilage will not regenerate. Unfortunately, the fibrocartilage which grows and covers these exposed areas does not have the same biomechanical properties as hyaline cartilage (fibrocartilage is denser and stronger in tension, while hyaline cartilage is spongier and stronger in compression) and it tends to wear much faster. Also, the height of the new fibrocartilage typically does not reach the normal height of the surrounding hyaline cartilage. Most consider these procedures only palliative or a temporary solution because hyaline cartilage is not being regenerated.
My advice, once again, is to consider these strategies very carefully. The “hopeful” benefits as well as the risks must be weighed, including the recovery and “down time.” Speak with your surgeon to make sure you are aware of all of the potential benefits and risks with regard to your particular diagnosis.
Also, if you are going to undergo knee arthroscopy, and you know you have arthritis in the joint, then I encourage you to discuss with your surgeon how these arthritic lesions will be treated. If arthroscopy is being performed to treat a problem in the knee, which is causing mechanical symptoms separate from the arthritis that is also present (for example, a meniscal tear), find out if the arthritic lesions will be ignored (which very well might be the best strategy) or if one of these techniques also will be used to treat the areas of arthritis. If the lesion is treated with drilling, abrasion or microfracture, then your postoperative rehabilitation might be more extensive and difficult, including not bearing weight on that lower extremity for a number of weeks. If treating an arthritic lesion proves to be the most appropriate strategy, it’s best to plan ahead for the after-care and rehab. Similarly, if you are to undergo hip arthroscopy, I think a discussion regarding how any arthritic lesions will be handled also is appropriate, because patients routinely are asked to limit weight bearing for a number of weeks following hip arthroscopic repairs.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.