Misconceptions about Partial and Total Knee Replacement
Recently, former President George W. Bush underwent partial knee replacement surgery, which has sparked a lot of media conversation, some of which I feel has been inaccurate and misleading.
Before considering knee surgery, you and your surgeon must carefully weigh the benefits of partial versus total knee replacement. Although age and physical activity play a role in the decision-making process, by far the most important consideration is the condition of the knee joint.
First and foremost, partial knee replacement (PKR) is beneficial for several reasons but only if there is symptomatic degeneration in one of the three knee compartments. During PKR, only one problem area is resurfaced, the implant is much smaller and only the bone and unhealthy soft tissue within that compartment are reconstructed. Many patients report that after PKR their knees feel more “normal” or “natural” compared to patients who have total knee replacements (TKR). While I agree that PKR might be underused as opposed to TKR in the U.S., I take exception that PKR is only for the young and fit, those who are not overweight or those who are in perfect health and are eager to get back to sports such as biking, running and even skiing. PKR surgery might be the optimal choice for a patient, whether young or old, big or small, physically fit or not, as long as the conditions are right.
A classic article by Kozinn and Scott, which still is quoted, was published in the prestigious Journal of Bone and Joint surgery in 1989 and described guidelines for “appropriate patient selection” for PKR. These included a patient’s age, more than 60 years old; weight, optimally 180 pounds or less; minimal pain at rest; range of motion, more than 90 degrees; flexion contracture of no more than 5 degrees; and any angular deformity which is less than 15 degrees and is passively correctible, i.e., the abnormal angle of the limb (bowlegged or knock kneed) can be corrected manually by the surgeon during the examination. With strict adherence to these criteria combined with better prosthesis and techniques, many centers have reported excellent long-term success.
In today’s world, many surgeons, including me, have challenged some of these classic criteria. It is remarkable how far the pendulum has swung, considering some individuals tout PKR only for the young and very fit who wish to resume athletics after surgery. This shift has been fueled by the confidence we’ve obtained from a larger and longer-documented collective experience with PKR, combined with better prosthetics and advances in technology to implant them. For many patients outside the “classic criteria” group, we’ve found that they have had success with long-lasting constructs that allow them to function at a very high level.
As we age, we are more prone to developing osteoarthritis in our joints, one of the most common causes for knee replacement surgery in adults. However, not everyone is afflicted with arthritic joint deterioration. I have successfully performed PKR surgery on many older patients and on patients who are not all that active but lacked the mobility to enjoy everyday life, and they’ve done beautifully. In addition, I also have performed PKR on remarkably active individuals, both young and old, and they too have reported excellent results and the ability to return to a very active and athletic lifestyle.
I also take exception that TKR surgery is only for older adults. Not true. Again, the decision to have PKR or TKR surgery depends on the person’s symptoms, how many compartments of the knee are damaged, the degree of knee deformity, the range of motion and if the deformity is correctible. TKR allows surgeons to correct much more severe deformities and defects than PRK. When done well and for the correct indications, both TKR and PKR relieve pain and allow an individual to a return to a remarkably high level of activity, if that is the goal. Both surgeries also can help patients remain independent and pain free, which is most often the primary goal.
A study from the United Kingdom recently was cited as indicating that death rates after TKR were four times higher than PKR due to a higher risk of post-operative complications. This is not surprising because TKR is a more extensive surgery with a more challenging recovery, so it is associated with an increased complications risk. Please keep in mind that while the rate for TKR may be four times higher, the rate still is remarkably low. According to the American Academy of Orthopedic Surgeons (AAOS), serious complications occur in less than two percent of patients undergoing TKR. The 30-day mortality rate for TKR is about one in 400, or 0.25 percent. That means that 99.75 percent of patients survive the treatment.
Researchers in the UK recently reported in The Journal of Bone & Joint Surgery that among 2,428 total knee replacement patients over a 10-year span, 99 percent survived at least one year. Those who did not survive might have died for any number of reasons not even related to TKR surgery.
I believe the key to minimizing the risk of complications for patients who undergo PKR or TRK lies in a careful and thorough evaluation prior to the procedure. If a condition exists that could increase a patient’s risk, such as heart disease or diabetes, then that condition should be fully assessed pre-operatively to see if it can corrected or improved. If it can’t, then it must be fully managed both during and after surgery. As a treating surgeon, by understanding what pre-operative conditions might increase risks post-operatively, I can customize treatment both intra-operatively and post-operatively to minimize these risks. This greatly decreases the chance of surgical complications and optimizes overall results.
In my experience, surgery that is expertly performed in a timely manner with the least amount of soft tissue trauma also makes for a smoother recovery. Expertly administered anesthesia, which in my OR often is regional, also decreases the risk of post-operative problems.
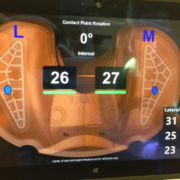
Computer Assisted TKR with the use of the VERASENSE OrthoSensor and Robotic Assisted PKR (Makoplasty) have been game changers for surgeons because they vastly improve the accuracy and reliability of performing these surgeries. Among the advantages, patients are assessed continually during surgery according to their individual anatomies. With use of on-going computer analysis in real time during surgery, it allows surgeons to make more accurate adjustments to achieve optimum prosthesis placement and more precise balancing.
Also noteworthy is that there have been significant improvements in the design of prostheses for both PKR and TKR. As we’ve gained insights into subtle knee anatomic variations and kinematics, prosthetic designs have been modified to reflect these insights and the results continue to more closely match the natural knee, including increased function and stability. Today’s implants are more individualized for each patient’s unique anatomy. In my practice, I choose the implant that is best suited to each person’s medical and lifestyle needs.
Throughout my 25-year career, I’ve seen patients with complex knee problems of all types including familial osteoarthritis, avascular necrosis, joint and bone destruction from past trauma, bad outcomes from prior surgery, infection, rheumatoid or other inflammatory arthritis, or childhood diseases.
As a surgeon, I must stress that each case is unique and the decision to have PKR or TKR surgery should be made only after a careful diagnosis and recommendation by your doctor. Correctly assessing which surgery is best for a patient is critical to a successful outcome.
As with all surgical procedures, it is imperative to choose a surgeon with a proven track record in this specialty. Get to know and have confidence in your doctor. Feeling comfortable with your surgeon will have a positive impact on your overall surgical experience.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.