Using Sensor Technology to Diagnose and Precisely Correct TKR Failures During Revision Surgery
In the last of three blog posts on the topic of unsatisfactory results post-TKR (total knee replacement), I will discuss using kinematic sensor technology to help me more precisely diagnose and correct a painful TKR.
Approximately 20 percent of patients who undergo TKR report that they are not satisfied with their results. Many patients go from doctor to doctor looking for answers and are told that their TKR looks “perfect” on the X-ray, and they “walk well.” Still, they aren’t happy. We call this the “looks good but feels bad syndrome.” Sadly, it’s all too common.
Approximately 40 percent of premature TKR failures that require revision surgery are due to component malrotation, malalignment and/or soft tissue imbalance. For the last two years, I’ve shared my experience using the Verasence Knee System to diagnose and help direct treatment for this group of painful TKRs at the American Academy of Orthopedic Surgeons’ annual meeting. This sensor technology allows me to diagnose a specific problem or problems that have resulted in failure (i.e., an unhappy patient) and provides data to help me correct it. This is proving to be very powerful. It’s comparable to how an automobile mechanic diagnoses a problem with a car. He or she plugs a computer into the car’s computer to check multiple systems to identify the specific problem in need of repair. I now do something similar to diagnose and fix a painful TKR.
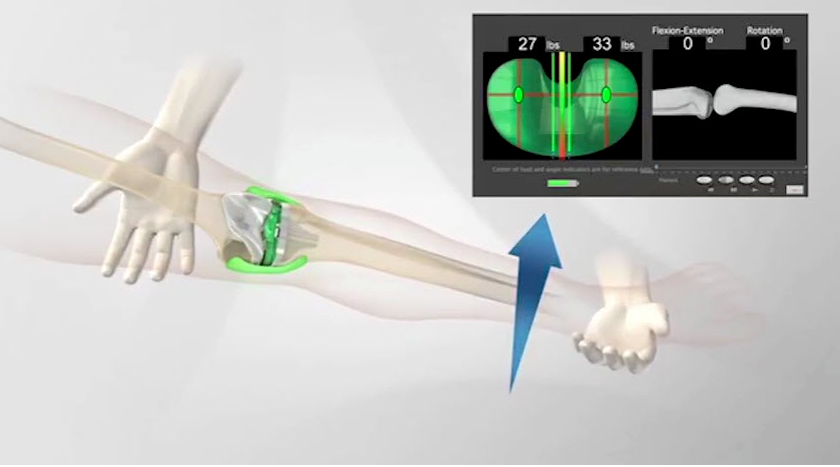
First, I remove the existing tibial insert and replace it with a Verasence sensor. Then, I assess the congruency or rotational relationship between the tibial component and femoral component. If the tibial is malrotated relative to the femoral component, then either the tibial component and/or the femoral component is not optimally positioned and must be changed. If this malrotated condition is observed, then femoral component stability, placement and rotation is verified. Accessing femoral rotation is accomplished by palpating small boney projections (epicondyles) medially (inside) and laterally (outside) on the femur which match the femoral epicondylar axis and must match the axis of femoral component. If malrotation exists, which is common, then tibial rotation is more often the culprit. My experience with balancing primary total knees using the Verasence Knee System has given me a much stronger appreciation for how small changes in the rotation between the tibial and femoral components result in major changes in the pressure or tensions experienced in the collateral ligaments. If the rotational relationship between the tibial and femoral components is less than desirable, due to tibial component malrotation, I remove and reposition a new tibial tray using the sensor to direct optimal rotation.
Once optimal femoral/tibial component congruency is created and/or confirmed, the knee is placed through a range of motion capturing inter-compartmental pressure measurements at various positions or poses. These pressure measurements correlate to inter-compartmental loads and ligament tensions and direct the balance of the medial and lateral collateral ligaments. Using this data, I select a plastic insert of optimal thickness to balance the soft tissue sleeve. Often, balancing the supportive soft tissue sleeve requires releasing part of the collateral ligaments medially or laterally. Usually, only select fibers within the ligament require release. Each time a small correction is made, I reinsert the sensor and generate new pressure measurements, thereby fine-tuning the balancing process. In the revision setting, the posterior cruciate ligament usually is removed or already has been removed during a prior surgery. This is a crucial structure which requires balancing when implanting a cruciate retaining TKR prosthesis, a type commonly used in a primary setting.
A major advance in our ability to revise total knees has been the availability of much broader prosthetic systems comprised of many more sizes and options. Today, total knee systems are modular and designed to allow the surgeon to build a knee from a huge assortment of parts to customize the prosthetic for each individual patient’s needs. Most total knee systems today provide different degrees of internal constraint, a variety of stem thicknesses, lengths and angles, and a variety of augments and cones. Still, revising a total knee typically is more challenging than performing a primary TKR. Special techniques often are required to expose the failed TKR and remove it. Sometimes, the surgeon must divide part or all of the quadriceps muscle or cut into the bone (osteotomy) of the upper tibial at the patella tendon tibial insertion to reflect it.
All too often during a revision TKR surgery the surgeon will change the entire prosthesis rather than only one or possibly two components. Although this approach can solve the problem, it doesn’t always, especially if the specific bio-mechanical abnormality that lead to the first failure was not addressed and corrected. Removing well-fixed total knee components (femoral, tibial, patella) requires special skill and instruments. For example, I use an ultrasonic instrument that vibrates at 70,000 times per section to melt through the cement-prosthetic interface to loosen the components.
Patience also is required because significant bone loss and fracture can occur during the removal process. If a component does not need to be removed in order to solve a problem, it’s much better not to. With the data generated by using the Verasence Knee System, I’m more often able to rebalance a failed TKR without removing all the components. This is new technology and is not available for all manufacturers’ prostheses at this time, especially older models.
Sometimes, even when the specific etiology for the failure is defined, it still is necessary to remove the entire prosthesis. For example, if I’m revising a knee with an older prosthesis and replacement parts are not available or adequate to solve the problem, I must remove the entire prosthesis. Many times, when revising a failed total knee, the surgeon will choose a tibial insert that interacts with the femoral component in a more positive or constrained fashion than was used in the primary knee. By doing so, the new prosthesis imparts more of the needed stability and the natural soft tissues which normally support and control the motion of knee are depended on less. Remember, these structures often are compromised or no longer present in the revision setting.
The downside is that with increasing levels of internal constraint, more internal forces are subjected to the prosthesis and the prosthetics attachment to bone. This is the trade off. If the prosthesis that is being revised doesn’t allow for this needed increased internal constraint, then again, complete removal may be necessary.
TKR is a game-changer and can make all the difference in a person’s quality of life. The vast majority of patients who undergo TKR are very grateful and satisfied. If someone has had a TKR and is not happy, there are definite solutions and logical ways to evaluate what the problem is and how to fix it. At The Leone Center for Orthopedic Care, our goal is to give each patient the best possible outcome, which begins with the first interview and patient examination.
Talk with your surgeon and let him or her know what your goals are. Understand what your treatment options are. If you truly have exhausted all non-surgical treatments and your knee is interfering with your life and well being, then TKR may be the most appropriate treatment option. I tell my patients that optimum TKR results require a partnership – 50 percent me doing a great reconstruction and 50 percent them putting their all into the post-surgery rehabilitation. If you’ve had a TKR and are not satisfied, I would recommend finding a surgeon who can help you define why your knee is not doing well so a plan can be formulated to improve it.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.