A Bad Total Knee Is Restored with the Use of an OrthoSensor Device
On June 29, 2016, I performed a really eloquent operation on a 55-year-old elementary school teacher from Nassau, Bahamas. I was so excited with how the case worked out for her that I decided to share the experience in a short blog.
She had traveled to America two years prior and underwent a total knee replacement (TKR). Unfortunately, despite her effort, as well as others involved in her care and extensive physical therapy after surgery, she did poorly and experienced continued pain and a poor range of motion (ROM).
When I met with her, she limped, could walk only a short distance and complained of serve medial knee pain. She was unable to fully extend her knee, lacking 20 degrees. This flexion contracture was even more disabling considering her non-operated, normal knee naturally hyperextended approximately 8 degrees and she could only flex her operated knee to 80 degrees.
After our initial appointment, I thought her incision had healed nicely and that her X-rays looked good. She was the “quintessential” patient that I described in a previous blog article discussing “The Unhappy Patient after TKR” who “looks good but feels bad.” She was frustrated, angry and the last thing she wanted to do was return to the U.S. for more surgery.
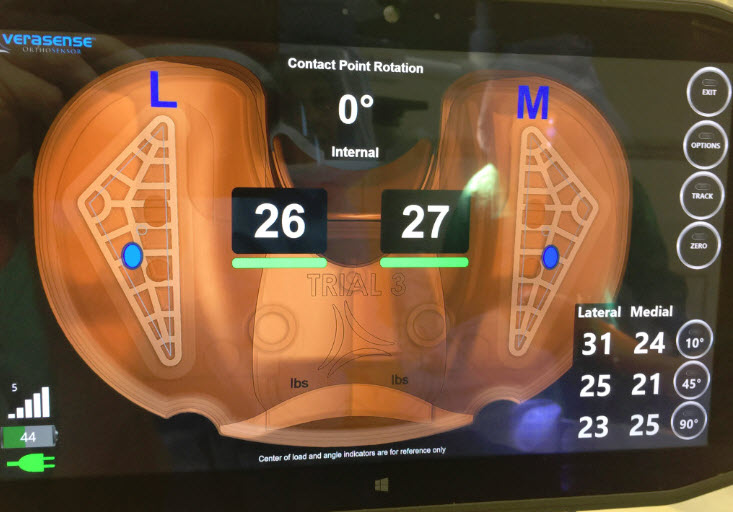
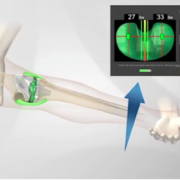
Preoperatively, her workup included aspiration of fluid from her knee, from which analysis revealed no evidence of infection. This was confirmed during her surgery. During surgery, I removed her plastic liner and inserted in its place an OrthoSensor device of the same thickness as the insert removed. I then measured her inter-compartmental loads (pressure measurements taken in both the medial and lateral compartments). This data allowed me to analyze the precise location and the amount of the pressures being generated throughout her limited ROM.
From this data, it became immediately clear that the tibial component was internally rotated 13 degrees relative to the femoral component. This degree of malrotation between the femoral and tibial components had a significant effect on the supportive surrounding soft tissues, which balance our knees. The lack of soft tissue balance directly effects ROM and stability, and can result in pain.
Normally when our knees move, there is a complex interaction of flexion-extension combined with internal-external rotation. The soft tissues, which surround the knee, have evolved to support and guide the knee during this complex motion pattern. If the femoral and tibial components meet each other in a twisted, less-then-optimal fashion, the surrounding soft tissue sleeve can’t perform naturally. So, when the knee flexes and extends, a part of the supportive sleeve will experience too much stress while other parts not enough.
During this patient’s operation, I also observed that throughout her knee’s ROM, lateral forces were much higher than medial forces and were excessive. I observed that her posterior cruciate ligament (PCL) was present and functioning appropriately, that her femoral component was appropriately sized and implanted and that the patella button was not an issue.
Based on these findings, I removed her internally rotated tibial tray, recut the upper tibia taking into account the excessive lateral pressures I had observed and then placed a new tibial tray. New data generated by using the OrthoSensor insert directed optimal tibial rotation relative to the femoral component. I also subtlety lengthened the lateral collateral, using a pie-crusting technique to further address lateral tightness. When this was completed, everything just fell into place. The knee’s ROM became full, inter-compartmental pressures balanced out perfectly and the PCL remained balanced. Wow!
I recognize that without this data, I would have done what is most commonly done in a revision setting like this, which is to revise both tibial and femoral components and increase the level of internal constraint. I avoided the “take everything out and start over” mentality because I had quantifiable data (the pressure measurements) which allowed me to precisely diagnose the problems with her first TKR and then specifically address and correct them. I literally performed her surgery yesterday and reviewed her postoperative X-rays just prior to writing this blog. Her X-rays looked like a first-time TKR with primary components. I consider this a wonderful and elegant solution.
I saw my patient the morning after surgery for her first post-op visit. She told me she felt good and was all smiles. I’m excited for her and anticipate she will recover even more quickly than a typical primary TKR patient because I did a lot less surgery. My hope and belief is that this will be a very different experience than her last.
I saw her again two weeks after her surgery. She expressed her gratitude, was walking without a limp and no longer using a cane. Her motion had improved nicely, but still is less than we both are hoping she’ll eventually achieve. She now fully extends but could flex to just 100 degrees. She has returned to the Bahamas and will fly back in a month-for re-examination. We discussed the possibility of manipulating her knee while under anesthesia with the goal of disrupting scar tissue, hopefully to improve final motion if her ROM is not acceptable at that time. I doubt it will be indicated. She seems very happy and motivated to continue rehab and to reach her full-function goal.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.









I am 79 years old and had knee replacement about 10 years ago. I have been to many doctors for consultation and was told not to do anything. I am in pain all the time and my walking is affected. I also broke my femur in five places and have a bar with many screws. Most recently I had two stents put into two anuerisims behind the knee in question. I have just about given up when I saw your ad. Do you think there is even a chance that you can help me. Awaiting a reply. Walter Srour
Dear Walter,
I don’t know if I can help you unless I better understand your history, examine your knee and study your X-rays. I see many individuals who already have undergone TKR and are not happy with their results. In many of those individuals, I have been able to help them by precisely diagnosing what part or condition of the new prosthetic knee was not functioning optimally and then correcting it. Often, it has required a limited revision, for example simply changing the plastic insert and re-balancing the soft tissue sleeve or changing both the plastic and tibial tray and then re-balancing surrounding tissues. The OrthoSensor insert has been invaluable. In each case, I go into surgery ready to revise the entire knee with what is necessary to solve the condition. I don’t know if this technology will help you our not without first seeing your leg and gaining a better understanding of the situation.
It is important to understand if the femur fracture occurred before or after your TKR and if the bone healed anatomically or not, in which case forces across the knee may have changed. Also, did you ever do well after TKR, or have you suffered ever since your surgery? Or, did you only develop pain after the femur fracture? Infection always must be considered and ruled out. If it is determined that you do have a correctable problem and further surgery is being considered, then fully understanding the vascular supply to your knee/leg is critical. If surgery was to be performed, it would almost certainly be done without a tourniquet.
I wish you the best. Let me know if I can help you.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.
I had a right TKR 9/29/15. There is too much motion in my knee for it to be considered a stable joint. I have continuous swelling and pain. I am 61 years old. In great physical shape 5’6″ 140 pounds. I still cannot do stairs one leg at a time as my operative leg will not hold me. I did physical therapy for 6 months. I did everything I was told to do. I think the knee is not stable. Can you help me? Where are you located? What state?
Dear Vicki,
The description of your symptoms does suggest soft tissue sleeve instability which critically supports, stabilizes and guides the knee through it’s complex motion arch. If the soft tissues that surround the knee are not balanced, then many people complain of symptoms similar to the ones you describe. Other causes which can lead to or add to these symptoms include component instability (that is, femoral, tibial or even patella component loosening), component malrotation, and component malpositioning. All must be fully evaluated or corrected if not optimal.
I would suggest you discuss these concerns with your surgeon. If you are interested in having me evaluate you, I would suggest you contact my office directly.
I wish you well.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.