Joint Preservation Strategies to Delay the Need for Hip or Knee Replacement Surgery
In the first of several blog posts about hip and knee joint preservation, I will discuss the mechanics of these amazing joints that help keep us moving and the conservative treatments that can delay and possibly prevent the eventual need for partial or total joint replacement.
As we continue to live longer and lead more active lives, the wear and tear on both our hip and knee joints has become a focus of the medical community. According to The Journal of the American Medical Association (JAMA), total knee replacements in Medicare patients have risen by 162 percent over the past 20 years. In December 2012, The JAMA Forum — comprised of a team of journalists who provide daily news about developments in medicine — noted that the number of total knee and hip replacement surgeries is predicted to quadruple, reaching 4 million a year by 2040. And, these surgeries, especially knee replacements, are becoming more prevalent in younger patients, not just the elderly.
There are conservative and even preventative measures everyone can take to manage pain and delay hip or knee replacement surgery. To understand prevention, you must first understand the way these joints work.
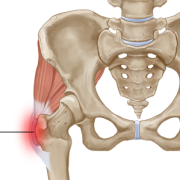
Hyaline cartilage is the tissue that covers the bones that come together in both hips and knees to form a joint. This highly specialized cartilage has unique wear characteristics that both help remove friction and distribute forces more uniformly throughout the bone. Unfortunately, when injured, hyaline cartilage heals poorly if at all. This is partially because cartilage does not have its own blood supply. The loss of hyaline cartilage results in arthritis.
Arthritis can be caused by a multitude of conditions, but the common result is the same: hyaline cartilage is lost. As more and more cartilage is lost, bones that make up the joint rub together, resulting in pain and joint inflammation and swelling. With time, the destructive process progresses until the pain and disability become so damaging that it impedes everyday movement and quality of life. At some point, the arthritic process becomes so advanced that less-invasive and more conservative treatment options no longer are not effective. That’s when join replacement surgery becomes a reasonable treatment option. Fortunately, joint replacement surgery has a wonderful track record of relieving pain and allowing individuals to become active again. However, everyone wants to cure or at least minimize discomfort and disability with alternative methods, while gracefully delaying the need for joint replacement.
At the Leone Center for Orthopedic Care, I see all types of complex hip and knee problems and my first advice to anyone is to learn about and understand the condition that is causing the pain. If an arthritic joint has developed, then it’s important to understand the condition or mechanics that lead to the arthritis. No matter what the cause, the next step is to develop a strategy to treat and if possible cure the condition, while preserving the joint with the least-invasive but most-effective method possible. I encourage my patients to “listen to and know their own bodies” to help preserve their joints. If you are experiencing continual or repeated intermittent pain, if knee or hip pain keeps you awake at night, or you experience pain when bending or rising from a sitting position, don’t ignore these signs. Seek advice from your doctor for a diagnosis and a treatment protocol that is right for you.
Some of the most common preventative and conservative treatments include:
- Exercise and physical therapy often are the first line of defense because damaged joints actually can worsen without movement. Although it’s difficult to move when you are in pain, a regimen with specific exercises tailored to your condition can help restore function and ease pain. In addition, physical therapy can increase a joint’s range of motion and strength. Pay attention to activities that seem to make the condition worse, as well as those that don’t. Consciously avoid those positions or activities that aggravate or cause pain. The mantra “no pain, no gain” simply doesn’t apply when trying to nurse and prolong arthritic joints. Likewise, if the physical therapy is aggravating and making the condition worse, stop. Many of my patients benefit from exercising in a pool, walking or swimming to maintain mobility and strength without “beating up” their joints.
- NSAIDs, anti-inflammatory drugs such as ibuprofen and naproxen, can help reduce pain and swelling caused by arthritis. Your doctor may prescribe a particular NSAID that delivers a larger dose or is taken less frequently. Long-term use of these drugs sometimes can cause undesired side effects, so it is extremely important that your doctor monitors this usage.
- Use of ice, massage, deep heat and occasionally nerve stimulation or ultrasound also helps.
- Glucosamine and chondroitin occur naturally in the body, but also are available as OTC supplements. Glucosamine aids in the repair of joint cartilage, while chondroitin helps to prevent other enzymes from breaking down joint cartilage.
- Weight loss: our joints carry the weight of our bodies and the more weight, the harder our joints have to work. Even small changes in weight make a significant difference in the forces on both our hip and knee joints.
- Some patients with knee arthritis obtain relief or an increased sense of stability by using an external knee brace or sleeve. Also, using a cane, walker or crutches can lessen the pain associated with walking or weight bearing from an arthritic knee or hip. For some, these devices also can minimize the risk of falling.
Intra-articular joint injections also are considered to be part of the arsenal of conservative treatments:
- Research indicates that some osteoarthritic joints have lower levels of hyaluronic acid, a naturally occurring acid found in the synovial fluid that acts as a joint lubricant. Some patients find relief from pain and stiffness with injections of hyaluronic acid that can last several months. However, it is not effective in all cases and does not stall the progression of arthritis
- Corticosteroids have long been used for symptomatic treatment for osteoarthritis. Corticosteroids, usually given by injection, provide joint pain relief by stimulating prostaglandin (hormone-like compounds) synthesis and decreasing the activity of collagenase and other destructive enzymes. Prostaglandins, unlike hormones, are not produced in a specific site but are found in many locations throughout the body. They act on target cells in the immediate vicinity of their secretion.
There is no evidence that intra-articular steroid injections slow the disease progression and their ability to treat symptoms typically weakens over a three-month period. Long-term use is not recommended because they can cause further joint destruction, as well as other side effects, including suppression of the immune system, elevated blood sugar and loss of bone calcium. Typically injections are limited to two to three a year and many surgeons discourage injections into a joint scheduled for surgery six to 12 weeks after the last injection.
Hylauronic acid injections also been used since the 1960s in an effort to restore the viscosity of synovial fluid in degenerating joints. Most of the common commercially available formulations are purified from the combs of chickens, and undergo chemical crosslinking to increase their viscosity and prolong their half-life. Typically, 2 ml are injected into the knee once a week for three to five weeks.
Once again, any realized effects are palliative in nature and if effective, the series of injections often is repeated. Because many formulations are derived from chicken combs, some individuals develop a sensitivity or allergy with repeat injections. Most common local symptoms include increased knee pain, swelling, redness and pain at the injection site. Occasionally, patients develop more systemic symptoms including fever, nausea, itching and headache which can mimic an infection.
There has been a wide range of reported outcomes. Recent clinical trials using meta-analysis, which combines the results from multiple studies in an effort to improve their accuracy, have demonstrated either no significant effect or significant improvement in pain and function. That taken into account, some patients report significant relief and request a repeat series when their symptoms return.
Patients need to be aware that it’s contraindicated to inject a steroid into a joint more than two or three time a year. Also, the therapeutic effects are almost always temporary. I have had patients refer to these injections as “band aids.” A steroid injection may not be appropriate for someone who has diabetes, advanced arthritis or has surgery planned within 6 to 12 weeks after the injection, due to increased risks of infection and tissue compromise.
Injections to the knee joint tend to be simpler and less painful than those to the hip. An intra-articular hip injection requires the assistance of fluoroscopy (which is like a moving X-Ray) or Ultrasound. Both methods allow for the visualization of the joint space to aid in more precise placement of the needle. It is not always easy, even with the aid of a fluoroscopy or ultrasound, to place the medicines into the hip intra-articular space because the hip joint space tends to be tight and there is significantly more tissue overlying a hip joint than the knee. In general, when a procedure has a greater degree of difficulty it carries more risk. If the initial injection of a local anesthetic combined with a steroid produces significant pain relief and increases joint function for three to four months, I think it’s reasonable to have it repeated, especially in the knee. I have further reservations with regard to repeating hip injections. Unfortunately, subsequent injections frequently will be less effective both in terms of pain relief and how long they provide beneficial results.
In my next blog, I will discuss treatments that specifically focus on treating joint osteoarthritis.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.