Soft Tissue Problems after Knee Replacement?
Should My Knee Still Hurt 1-2 Years After Total Knee Replacement?
What Causes Knee Pain Years After Knee Replacement?
Should you have soft tissue problems after knee replacement?
The short answer is no. If you have undergone a total knee surgery and you still have pain after healing, then my advice is to try and understand why you are having pain and not doing well so hopefully it can be fixed. Some patients take up to one to two years to see their full improvement. In this blog article, I will try and describe how to find out why your total knee replacement is not comfortable. Armed with the “why” or underlying etiology, then a strategy can be designed to fix it. Fixing the problem is a subject for a different article.
Total knee replacement (TKR) has been “no less than a miracle surgery” for the vast majority of the more than 600,000 people who have the surgery each year in America. To me it is “like a beautiful orchestra,” when all the moving parts perfectly align, pain is relieved, and function restored. But not everyone is always happy. Many studies report that 15 to 20 % of people who have had TKR are not satisfied with their result. The question becomes what is different between the group that is satisfied and the group that is not? And if those differences can be defined and repaired, can folks in the not satisfied group move into the “I’m satisfied” group? The answer in many cases is “yes.”
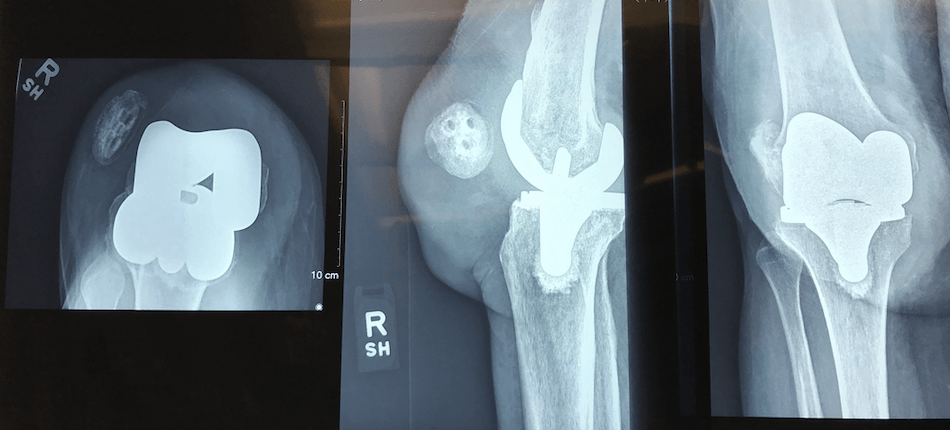
When someone undergoes a TKR, the goal of surgery is to realign the limb if it is angulated abnormally. Balance the surrounding tissue which help guide the knee through its natural motion. Resurface the femur, tibia and patella so bones no longer rub together (bone on bone) and metal surfaces now only touch plastic surfaces. And securely fix the implanted prosthetic components to the underlying bone. When all these variables come together perfectly, “like a symphony,” these tend to generate the best results with the happiest patients. When one or more of these variables or “goals” are not achieved, it often results in someone not being happy with their TKR.
(Note: I listed and expanded on some of these “goals when performing TKR” at the end of this blog article for anyone interested)
So, if you are someone who has had a TKR and you’re not happy with your result, how do you figure out what’s wrong so you can improve it? I suggest you start by returning to your surgeon and sharing your complaints and concerns. Hopefully, they can give you answers and clear direction forward. If your original operating surgeon is not able to help you further, then I suggest seeking a second opinion from another orthopedic surgeon. If possible, select an orthopedic surgeon who has special interest and knowledge in knee replacement surgery and specifically revision TKR.
When scheduling an appointment for that second opinion, it is important to bring your medical and orthopedic records which save time and are invaluable. In particular, bringing images (X-rays) of your knee taken before your knee replacement and soon after, as well as your operative note and implant record. The pre-operative images give me insight regarding any deformities you had prior to surgery and how they were addressed. Occasionally, the preoperative images show very little if any arthritic change or deformity and that too can give insight why someone is not happy with their result after TKR. Was the knee really the problem to begin with (consider referred pain for the hip or lower back) and were the goals of surgery realistic (i.e. running marathons)? The films also allow assessment of the implant sizes used to recreate your knee’s normal anatomy and relationships. Early post-op images allow comparison to very recent images (I typically take new X-rays). I look for a change in component position, alignment and the contact area between the prostheses and the supportive bone (bone prosthetic interface). Changes can provide big clues as to what’s going on, i.e. component loosening, subsidence or lack of soft tissue balance. The operative note and implant record allow me to understand the operating surgeon’s diagnoses and then how they attempted to fix it. The implant record names the exact company who made the implants along with the implant’s brand name, size and tracking number. Some implants have performed much better than others. Many patients who I see for further opinion have already had other second opinions and any work up or studies already done again are invaluable. If past blood work was done, bring it. If special studies were done, like an MRI or bone scan, bring them. If the knee was aspirated, definitely bring all of these results.
When I see someone for a “second” opinion regarding their TKR which they are not happy with, I start with a thorough history. Often, this history will give specific clues to why a TKR is not functioning well.
Infection always has to be considered and hopefully ruled out in any patients who has a painful TKR. Many TKR that are infected don’t necessarily “look infected” and making this diagnoses is often difficult. Many infected TKR don’t necessarily look “hot and swollen”. Very seldom will someone with an infected TKR develop fever and chills. The incisions often look healed and unremarkable. Then what are the clues? Possibly, a history in which there was prolonged wound drainage after surgery or difficultly with the wound healing. I inquire if antibiotics were continued or restarted after surgery and if they returned to the operating room for additional surgery? Patients who report that they never did well also are more suspicious for infection, although infection can also start later.
Some conditions increase one’s vulnerability to infection such as diabetes or peripheral vascular disease. Patients who are immunocompromised (i.e. Rheumatoid arthritis) or who take medicines that compromise their immune system (i.e. chemotherapy, biologics, HIV meds) are more vulnerable to infection. Patients who are significantly overweight or who smoke also are more likely to develop an infection. An infection elsewhere in the body such as the mouth (root canal) or urinary tract (UTI) can lead to a TKR infection. Knowing this information is critical in my “detective work” when trying to determine why someone is not doing well after their TKR.
To assess if infection is present, I routinely ask patients to have blood drawn for ESR and CRP, if it has not already been done. These studies measure sensitive inflammatory markers that many times are elevated when there is an underlying infection, but they are not specific just to infection. If these studies are elevated, then fluid from the knee is removed (aspirated) for study and culture. Sometimes my “index of suspicion” is high based on their history, or appearance of the knee or X-rays, I will aspirate fluid even before the blood studies have returned.
The character and timing of the pain/discomfort also give clues as to whether there is an underlying infection. Rest pain (meaning pain occurring without movement or weight bearing), pain that awakens someone at night, and constant increasing awareness or discomfort, are all consistent with infection though sometimes these classic symptoms are not present or present without infection.
Knees that are only painful with movement or weight bearing and not at rest suggests a mechanical etiology. A knee prosthesis that is loose (not securely fixed to the bone) will move or “toggle” a little, especially during weight bearing and can cause pain. A TKR which feels “too tight” or “too loose” leads to a compromised range of motion or an abnormal motion pattern with resulting pain from irritation and often an overload of soft tissues with inflammation and pain.
Sometimes X-rays allow us to diagnose a loose component but many times they do not. Bone scans and MRI scans also often don’t allow us to definitively diagnose loosening. Comparison to earlier X-rays looking for change is one of the best ways to see subtle change. Recognize that infection can also lead to loosening of a component.
As a clinician, I often rely on the patient’s description and location of their pain. Their history often prompts me to have more X-rays taken or consider a diagnostic injection with a local anesthetic as a test. A steroid usually is not injected unless the diagnosis is known and I am trying to treat a specific problem. If a component is loose and pain is caused with weight bearing or walking, then many times a local injection into the knee will relieve all their pain temporarily. I can also temporarily relieve pain from other etiologies inside the knee joint space as well as a loose component, so while this test is not 100% specific for loosening, it does add to our understanding the etiology of the pain. Remember, the painful or “not satisfactory” TKR condition can’t be addressed and corrected unless the etiology is fully understood.
Many patients report a tightness or “band like” / “vice like” discomfort around their knee. Many times, this is associated with less than optimal soft tissue balancing, resulting abnormal knee kinematics (movement) which results in pain from abnormal soft tissue stresses. Pain can also result from total knee components that are too big or too small, again often resulting in abnormal knee kinematics. If the femoral and tibial components do not touch (articulate) each other in the optimal relationship (i.e. too much tibial or femoral internal or external rotation), knee movement is effected and again can result in abnormal stresses in the soft tissues with pain and instability.
Many times the “looks good but feels bad” total knee falls into this category which I’ve written about before. The leg looks straight, the incision healed nicely, there is no indication of infection, the patient achieved a satisfactory range of motion but they are unhappy with discomfort and that limits their ability to be active. Many times their symptoms are from subtle imbalances in their soft tissue sleeve with or without less than optimal component positioning that accounts for their symptoms.
A physical exam often gives powerful clues to underlying etiology. I observe how someone gets up after sitting and walks and then exam their knee. Do they use their arms to help them arise to take pressure off the affected knee? Do they avoid initial pressure to a particular side? Do they hesitate or delay before starting to walk? Sometime patients will tell me they are letting their knee “get into position.” Are they limping and how do I characterize their gait pattern? All give clues to the underlying etiology.
Thoroughly examining their knee and comparing to the other side is critical. Is the knee swollen and hot? What does the incision look like? Is the knee draining? Is there weakness? What range of motion did they achieve? Sometimes when I see a remarkably full range of motion it’s a clue that the soft tissues are too loose. Sometimes when the range of motion is very restricted, it also suggests another possible underlying problem. Is the knee balanced when it is stressed in different planes or does it “open up” or “translate” which may suggest instability? Does the knee “wobble” and “make noise” when the leg is dangling? Is the patella tracking centrally or tracking off to the side? These are all clues.
Examining both hips and knees are also important as well as their back, neurologic exam and vascular exam. I feel like a detective looking for clues and trying to put it all together.
The vast majority of folks who undergo total knee replacement are very pleased. Unfortunately, some are not. If you fall into the latter group, then systematically and methodically evaluating your TKR often exposes why your result is not acceptable. Armed with a clear understanding of “what went wrong” a strategy can be created to try and address any issues and correct them. Revising a failed TKR is not as predictable as operating on someone for the first time. (again, the subject of a different blog article) But if you are unhappy enough, i.e. benefits outweigh the risks, then many times having further surgery is reasonable.
As promised, I listed and discussed in more depth the “goals when performing a total knee replacement” in the context of “figuring out what is wrong.” I realize this may be “too much” for some folks. When all of these conditions are optimal and satisfied, patients tend to have the most predictable and “perfect” results.
- Re-create the limb alignment that is similar to their natural alignment prior to developing a knee problem. Typically, this means straightening out a limb that has developed a bow leg (genu varus) or knock-kneed (genu valgus) deformity. Careful: if someone has always had some degree of bow leggedness or knock knee (we call this constitutional varus or valgus), and after TKR if the limb was made perfectly straight, that may help explain why their TKR is not comfortable for that particular patient.
- Re-create the natural tension or loads on the supportive soft tissue sleeve throughout the knees range of motion. This soft tissue sleeve is made up of ligaments and connective tissue bands which help guide the knee through very complex movements as the limb flexes and extends. This is critically important and not re-creating this complex knee motion can be a major source of dissatisfaction after total knee replacement.
- Re-creating normal knee “kinematics” or movement. With a healthy natural knee, the lower leg bone or tibia internally rotates as the knee flexes and externally rotates as the knee extends. Or to say it another way, during flexion the outside or lateral aspect of the femur (lateral femoral condyle) moves backward or posterior on the tibia, to the point of actually “falling off” the back of the tibia when fully flexed. The inside of the knee or medial aspect of the femur moves backward just a little during flexion. During extension or when straightening one’s leg, the opposite occurs as the tibia externally rotates and moves back under the lateral femoral condyle or outside bottom of the femur. So in essence, there is rotational movement as the knee flexes and extends, pivoting on inner aspect of the knee or medial compartment. This is referred to as the “screw home mechanism.” The closer the TKR mimics this natural movement, the more physiologic the tensions in the soft tissue sleeve that is guiding this movement and the more comfortable the patient is with their total knee.
- Re-creating an optimal relationship between the resurfaced femur and tibia is also critically important to create optimal kinematics and a comfortable TKR. If the rotational alignment between the tibial and femoral components is off, this can result in their supportive soft tissue sleeve feeling “twisted” preventing normal knee kinematics and result is discomfort and sometimes instability. Patients often complain that their knee does “not feel stable” or “feels tight” and is uncomfortable.
- The components implanted must be stably mounted to the body’s skeleton. Remember, TKR is a resurfacing operation. We re-surface the ends of the femur, tibia and underneath surface of the knee cap (patella) so only metal surfaces touch plastic. Whether the components are cemented or press-fit, hoping to achieve stability with bone in growth, if there is movement or “toggle” between the prostheses and bone, it can create pain and a poor result.
Click here to read or watch videos of the many grateful patients of Dr. Leone.
The Leone Center for Orthopedic Care at Holy Cross Health is located at 1000 NE 56th Street in Fort Lauderdale. For more information or to schedule a consultation, please call 954-489-4575 or visit holycrossleonecenter.com.