Revision Hip Replacement Surgery
Revision hip replacement surgery refers to more hip surgery being performed on a hip that already has a total hip implanted. Typically, a “revision” hip replacement surgery is a more complex procedure requiring more operative time, expertise and special equipment. The potential complications associated with revision surgery also tend to be greater. Removing the old prosthesis can be destructive and often requires a more extensive incision and dissection. Fortunately, revision surgery has become much more reliable and reproducible with the development of specialized instruments and techniques. Modular prosthetic hip implant systems with bone ingrowth surfaces have been developed to perform these complex re-do surgeries with major bone deficiency much easier and more satisfactory than in years past. . These have vastly improved our ability to reconstruct the hip and still achieve an excellent and predictable result.
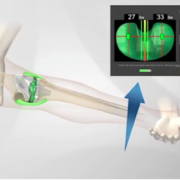
Hip Dislocations or Instability: There are multiple reasons why a person who already has a total hip, would require more surgery. One of the most common reasons is instability. The prosthetic ball dislocates from its intended position in the socket. Critical to reconstructing a stable hip with equal leg lengths is implanting the cup and stem in an optimal position in the bone and with respect to each other. In my experience, the pelvic alignment level (PAL) (visit the Video Gallery to view the PAL video) has been essential in my ability to accomplish this consistently. The size of the femoral head, which is typically being implanted today compared to just several years ago, is larger. Larger femoral heads are more stable than smaller ones. This has been possible because on a molecular level, the quality of the plastic bearing surface has been improved. By increasing the polyethylene cross-links while eliminating oxygen free radicals, the bearing surface is made much more resistant to wear. Alternate bearing surfaces have also been developed including those made of ceramics and metal. In spite of the strategies that have been developed in recent years, instability is still a major reason why some total hips need revision.
Loose prosthesis and Osteolysis (bone loss): Another common reason why revision surgery becomes necessary is due to the bone that is supporting the prosthesis becoming deficient or absent. This can lead to the loosening or instability of components. After millions of cycles and years of use, the prosthetic ball wears into the socket. Tiny particles of debris are produced which incites an inflammatory response and stimulates the resorption of the bone that supports the implants. This condition is called osteolysis. It remains one of the biggest problems with any joint replacement in the body. Better quality plastics and alternate bearing surfaces have been developed with the hope of diminishing osteolysis. Highly cross-linked polyethylene which is being implanted in most modern prostheses and in revision surgeries has greatly decrease the incidence and amount of osteolysis occurring compared to years prior.
Infection, fracture around the prosthesis, and leg length inequality are other common reasons why a revision or re-do surgery becomes necessary.
Metal on Metal Bearing and Corrosion:
Historically, controversy existed regarding the optimal bearing for the total hip. Today, most consider a ceramic ball articulating against a modern “highly crossed linked polyethylene” socket to be the “gold standard”. Traditionally, a metal ball attached to the stem was implanted and articulated against a plastic cup. Many different bearing have been studied with the hope of improving the longevity of the joint by improving the wear characteristics between the ball and the socket.
Many patients world-wide were implanted with “metal on metal” bearing. That is, a metal ball moving against a metal liner. These condition were created in the standard THR and
Hip Resurfacing (HS). Hip resurfacing involves implanting a metal cup directly into the pelvis and covering the reshaped the arthritic femoral head with a metal cap. Both conditions are created so that a metal ball will articular against a metal liner.
Theoretically and in a laboratory environment, a metal on metal articulation has the potential to produce less friction and produce less wear than standard metal balls moving against a plastic liner would. It requires fluid to exist between these two surfaces acting as the lubricant, called fluid film lubrication”. It also requires that the ball and socket are perfectly positioned and manufactured. Also the patient must not exceed the mechanical limits of the joint. If any of these conditions if not present, the lubricating fluid breaks down and them metal surfaces rub together (edge loading) creating metal debris and problems.
Many patients with metal on metal THR or HR world-wide are now experiencing problems that require revision. The high concentrations of metal ions can destroy tissues locally and are resorbed systemically which can cause a host of problems. Because some of these patients remain asymptomatic until the destruction becomes extensive, it is important to proactively look for potential problems with baseline studies and have more regular follow up than standard metal or ceramic on plastic articulations. If problems are developing it is better to revise their hips sooner rather than later to minimize soft tissue destruction. In my practice I’m seeing many more patients with metal on metal articulation with problems.
Modular ball and stem with Taper Corrosion: Historically, the metal ball attached to the femoral stem was made from a single piece of metal. Now, almost all stems that are implanted world-wide are “modular”. That is, the ball is separate from the stem or “modular”. Modularity helps the surgeon can more easily “fine tine” hip mechanics and leg length by choosing from balls with different neck lengths and sizes. Because cup plastic quality is so much better than it was years ago, larger diameter balls are being implanted on the tapers of these modular stems, which has the advantage of improving stability and lessening dislocation. We are now seeing more patients present with corrosion developing between the taper and the ball (taper corrosion). Metal corrosion products leach from this taper-ball junction and can also lead to local tissue destruction and problems systemically. They too require revision.
While the reason why this is occurring appears to be multifactorial, it is being intensely studied and debated. We know it is creating very serious problem for some patients. It is also a potentially very large clinical problem worldwide because so many individuals have modular head neck junctions.
Modular neck stems and corrosion: Modularity was taken a step farther, again with the hope of giving the surgeon more intra-operative flexibility to optimize hip mechanics, leg length and stability by also making the neck of the stem modular. Usually the neck with taper and body of the stem are all made out of one piece of metal. Experience has shown that this class of primary hip stems has done poorly and a large per cent have required revision. Some have even been recalled by their manufacturer.
Infection also remains a reason why some THR require more surgery. Every effort is made to prevent a total joint from getting infected because treating if is so difficult. The treatment requires surgery. Antibiotics are also in conjunction with surgery. Antibiotic alone are ineffective.
If the infection is considered acute, that is it occurs the first several weeks after surgery and the infecting organism is one that is sensitive to antibiotics, then re-opening the hip, thoroughly and meticulously debriding and irrigating while removing and then replacing the modular ball and plastic liner, followed by IV antibiotic (typically for 6 weeks) and then PO antibiotics may salvage the artificial joint and result in a cure. It may also fail.
If the infection chronic, or includes several organism or involves a fungus or particularly resistant organisms, then it requires a two stage re-operation to treat and hopefully cure the infection. The first re-operation involves removing the total hip prosthesis, again extensively and meticulously debriding and irrigating and then placing a spacer or temporary total hip. The temporary total hip is implanted with large quantities of antibiotics added to bone cement and new components are re-implanted but provisionally, planning for the second stage in several months. This new total hip which we re-implant is referred to as a “dynamic spacer”. It allows the patient to walk and rehabilitate their muscles and tissues but is not definitive or as comfortable as the definitive total hip. IV antibiotics (typically for 6 weeks) and then often a short course of PO antibiotics are given before the second stage re-implant.
A second operation is then performed when the antibiotic courses are complete and pre-operative studies indicate that the infection cured. During the second stage surgery, the temporary total hip is removed, the joint is again irrigated and debrided and now definitive revision component are implanted. Antibiotics continue until intra-operative cultures are negative and sometimes longer.
Occasionally despite the fact that an infection has be present for a long time (chronic) or one of the other factors that would typically encourage treatment with a two stage operation, only a one stage surgery is practical. This may be the most appropriate strategy in a patient who is too medically frail or sick to undergo two major surgeries or in a person who has already had a revision surgery (and indeed the incidence of infection in revision patients is much higher than in primary THR) or multiple revision surgeries and if the prosthesis was removed it would preclude or greatly compromise the ability to re-implant another. In these circumstances, the joint is surgically debrided and irrigated, the modular head and liner are replaced with new ones, the patient is treated with IV antibiotics and then will remain on a suppressive PO antibiotic hopefully for life. The goal is to suppress the infection so it is not expressed, recognizing it is not actually being cured.
The best treatment for infection associated with a total joint is prevention.
These are just some of the reasons why revising a THR may be necessary. Critical to obtaining as perfect a result as necessary after the revision surgery is fully understanding why the existing hip failed, extensive preoperative planning, optimizing the medical condition of my patient both before, during and after surgery, correcting all the problems that lead to the failure and finally re-building a mechanical construct that is stable and re-creates hip mechanics. On a positive note, many of my revision patients are some of my most grateful patients.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.