Platelet Rich Plasma (PRP): A Biologic Solution – “Heal Thy Self”
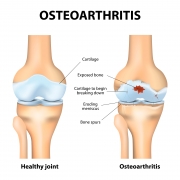
In my previous blog post about joint preservation strategies, I discussed conservative treatments that could delay or possibly prevent the need for partial or total joint replacement. I also touched on what arthritis is and what causes it. The common result of arthritis is the loss of hyaline cartilage.
When the arthritic process becomes so advanced in hip or knee joints that less-invasive and more conservative treatment options no longer are effective, surgery becomes necessary. Joint replacement is a wonderfully successful method to treat the condition, however it is definitive, non-reversible and should be utilized for “end stage” arthritis after others options are inappropriate or have failed.
In the next few blogs I will discuss different biologic strategies designed with the hope of delaying, encouraging repair or preserving arthritic joints to prolong or prevent the need for surgery.
Currently in the medical community there is an enormous interest and energy being focused on finding biologic solutions for cartilage regeneration to stop the progressive, ill-effects of arthritis. There are several exciting, new treatments to stimulate the regeneration of hyaline cartilage, which most commonly are being used for the knee. These treatments tend to be limited to small areas of cartilage loss, which often results from trauma or sports injuries, and are for patients who are in the earlier stages, and who do not have advanced osteoarthritis or damage. The great attraction for and goal of these treatments is to provide pain relief and hopefully stop or delay the arthritic progression by re-creating a normal joint milieu and activating the body’s own reparative mechanisms to heal.
One of the most pioneering strategies is Platelet Rich Plasma (PRP), an exciting new treatment option that is being applied to many musculoskeletal problems because of its potential to promote the healing of injured tendons, ligaments, muscles and joints.
Our blood contains platelets, highly specialized cells that do not have a nucleus and function primarily to stop bleeding. Platelets also play a key role in wound and soft tissue healing. The basic principle underlying PRP is to use concentrated platelet cells to simulate the body to heal itself.
PRP treatment consists of a high concentration of platelets with an associated large pool of signaling proteins (called growth factors and cytokines) delivered by injection into an injured area. The expectation is that these injections will turn on or stimulate (up regulate) the body’s own natural healing mechanisms. The hope also is that these proteins will alter the inflammatory mechanism and stimulate specialized cells to migrate to the injured tissue and multiply, as well as induce an increased blood flow needed for healing.
This high concentration of platelets is obtained by centrifuging blood drawn from the patient, who subsequently will receive the injections. PRP is combined with a local anesthetic and injected directly into the inflamed tissue or damaged joint. As with many injections, the patient may feel increased initial pain, which usually subsides slowly after several days. Hopefully, after several weeks, the initial discomfort associated with the arthritic joint or injured tissues improves. Because PRP is derived from a patient’s own blood, many consider it as safe as a cortisone injection. Although many more patients have undergone knee PRP injections – hence there is a much larger body of medical literature describing the experience – some patients also are undergoing PRP hip injections.
The medical community’s understanding of PRP is still in its infancy. Controversy exists regarding the optimal techniques to prepare the PRP, the medical conditions for which PRP injections are appropriate and effective, the amount to inject and even the appropriate number of injections. The exact mechanisms that lead to success as well as the definition of success still are being defined. Basic questions still must be answered with longer-term, well controlled studies.
My feeling is that this new treatment modality is exciting, but needs to be explored with caution and common sense, as well as optimism. If an arthritic joint already has significant deformity such as “bone on bone,” reactive changes such as spurs or degenerative cysts, or there are associated soft-tissue contractures, then the patient’s chance of having any real long-term relief from PRP treatment is extremely small or none at all.
Currently, PRP is being offered by a wide variety of physicians. PRP is not regulated by the FDA because it is derived from the patient’s own blood and is neither a drug nor an implant and it is often not covered by insurance because it is considered experimental. Therefore, for many patients who desire this treatment, they must pay “out of pocket.” In a time of diminishing reimbursements, this is a major consideration.
The general media has exposed many of us (both the general population as well as the medical community) to the PRP success stories of famous athletes and celebrities. While these reports are exciting and “make headlines,” they are anecdotal. We await the large, well-controlled, blinded studies on which science has come to depend.
I believe PRP offers great promise and in the future very well may have a definite, defined place in our armamentarium to treat diseased joints and tissues, but its niche is yet undefined. For now, while it offers hope, it feels much like the “wild, wild west” with extensive marketing and promises that are not well documented.
My advice to anyone contemplating PRP treatment is to speak with your orthopedic surgeon or healthcare provider and then carefully weigh the potential benefits and risks. The risks and out-of-pocket expenses should not outweigh the benefits.
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4575 or by email at LeoneCenter@Holy-cross.com.










Could PRP be effective with Hips or just knees and smaller joints?
How many cases have been successful for this alternative option
to total hip replacement.
Would you consider this treatment prior to hip surgery for an elderly lady (71)
with osteoarthritis. Thanks. Colomba Ghigliotti
Dear Ms. Ghigliotti,
The exact indications for PRP are still being determined. I would not expect a PRP injection placed in an arthritic hip, especially for someone who is 71 years old, to be an effective treatment. Fortunately, this condition can be treated very effectively and predictably with THR when the symptoms are disabling enough.
I wish you a full recovery.
Dr. William Leone
We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com. General comments will be answered in as timely a manner as possible.