The SPAIRE Technique
Most muscle-sparing and minimally invasive hip approach with no hip precautions
As my experience with the SPAIRE technique combined with a mini posterior approach for total hip replacement (THR) grows, so does my enthusiasm. I think it represents the “best of both worlds”. As I described the SPAIRE approach in an earlier blog article, unlike a standard posterior approach or even mini posterior approach, this technique does not release the short external rotator (SER) muscles which overlay the upper (superior) and back (posterior) position of the hip joint. With the SPAIRE technique, I develop the interval between the SER muscle group and underlying hip joint capsule. Only the single tendon of the obturator externus is released and is reattached after the hip replacement is complete with the quadratus femoris at its anatomic attachment. This creates an opening into the hip and looks like a trap door, inferioposteriorly, which refers to the bottom and back area of the hip.
One of the advantages of preserving the SER muscles rather than releasing them and then repairing is improved stability against dislocation. With a standard posterior approach or mini posterior approach without SPAIRE, until the repaired tissues heal, the individual is at increased risk for a posterior hip dislocation. For a posterior hip dislocation to occur, the hip typically impinges anteriorly (in front) which then levers the ball out the back. Because these anatomic structures are intact combined with a robust and anatomic repair of the hip joint capsule, the posteriosuperior position of the hip is no longer vulnerable and hence we’ve eliminated “hip precautions” such a sitting in low chairs or crossing one’s legs. Also, when the SER are repaired after releasing, they cannot be anatomically repaired to the original point of attachment like the obturator externus muscle.
Historically the short external rotators (SER) muscles were considered vestigial (once something very important, but no longer) in humans or to function as proprioceptive organs (send nerve electrical signals back to our brain in regards to where the hip joint is space) and to thicken the hip joint capsule. It is now recognized that the SER muscles are primary movers of the hip joint and assist other muscles that move the hip as well. They also act as hip stabilizers. 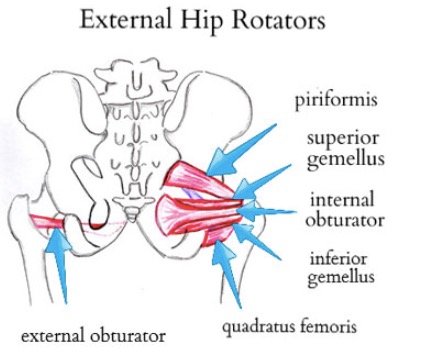 While anecdotal, I am routinely seeing patients return who I’ve performed double hip replacement, one replaced prior to my using the SPAIRE technique and the second with SPAIRE. They are telling me that their second hip “got well even faster” and “feels stronger sooner”. I recognize this is anecdotal and I don’t know if in the long run that preserving these structure makes a clinical difference, my impression is that in short term, it seems to and I’m much more confident encouraging patients to resume their full activities as soon as they’re comfortable doing so without specific precautions.
While anecdotal, I am routinely seeing patients return who I’ve performed double hip replacement, one replaced prior to my using the SPAIRE technique and the second with SPAIRE. They are telling me that their second hip “got well even faster” and “feels stronger sooner”. I recognize this is anecdotal and I don’t know if in the long run that preserving these structure makes a clinical difference, my impression is that in short term, it seems to and I’m much more confident encouraging patients to resume their full activities as soon as they’re comfortable doing so without specific precautions.
The Direct Anterior Approach (DAA) has been touted as the most muscle-sparing approach and patients are not asked to follow hip precautions after their surgery. Doctors are able to use a fluoroscope to help them get the components in an optimal position. There is a growing body of evidence showing there is no significant difference in the dislocation rate, component position, and post-operative gait recovery when using DAA versus a posterior approach for total hip replacement (THR). A significant limitation of the DAA is the need to release the superior (upper) hip joint capsule to facilitate femoral head delivery. This is performed from within the capsule and compromises the SER attachment and it is then impossible to perform a robust repair. Further, when patients have tight soft tissue structures or contractures, femoral exposure becomes even more difficult and requires more soft tissue release including the posture capsule to facilitate delivery of the upper femur for reconstruction. Because femoral exposure is difficult through the DAA, the implanted stem many times does not go down the middle of the femoral canal. Sometimes the end of the hip stem then touches the inner aspect to the femur at this level and results in pain.
Total hip replacement has been one of the most important operations developed in the past century. Reliably and predictably, patients do well when certain critical tenets of the surgery are met. This can be accomplished using a variety of prosthesis, approaches and by a variety of surgeons. As we exceed 50 years performing THR and each year attempts to improve this remarkable surgery, any technical advancement must demonstrate improvement in the functional aim of the procedure which is to relieve pain, restore anatomy and improve function. Any modifications which are made to the prosthesis or technique must also be able to be accomplished with minimal complications and the construct needs to last for many years. I believe the SPAIRE technique combined with a mini-posterior approach accomplishes these goals and allows for easy extension or enlargement of the incision and dissection should more exposure be necessary such as for a fracture. This is not the case with the DAA.
Click here to see the hundreds of testimonials from Dr. Leone’s grateful patients. These testimonials keep the team going strong every day.
Dr. William A. Leone is head of The Leone Center for Orthopedic Care at Holy Cross Health in Fort Lauderdale, Florida and has earned a reputation as one of the nation’s top orthopedic surgeons. An orthopedic surgeon with extensive experience, his specialty is solving complex hip and knee problems. We thank you for your readership. If you would like a personal consultation, please contact our office at 954-489-4584 or by email at LeoneCenter@Holy-cross.com.